
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Metabolic Risk/Epidemiology
- A Composite Blood Biomarker Including AKR1B10 and Cytokeratin 18 for Progressive Types of Nonalcoholic Fatty Liver Disease
- Seung Joon Choi, Sungjin Yoon, Kyoung-Kon Kim, Doojin Kim, Hye Eun Lee, Kwang Gi Kim, Seung Kak Shin, Ie Byung Park, Seong Min Kim, Dae Ho Lee
- Received June 18, 2023 Accepted August 16, 2023 Published online February 1, 2024
- DOI: https://doi.org/10.4093/dmj.2023.0189 [Epub ahead of print]
- 780 View
- 50 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
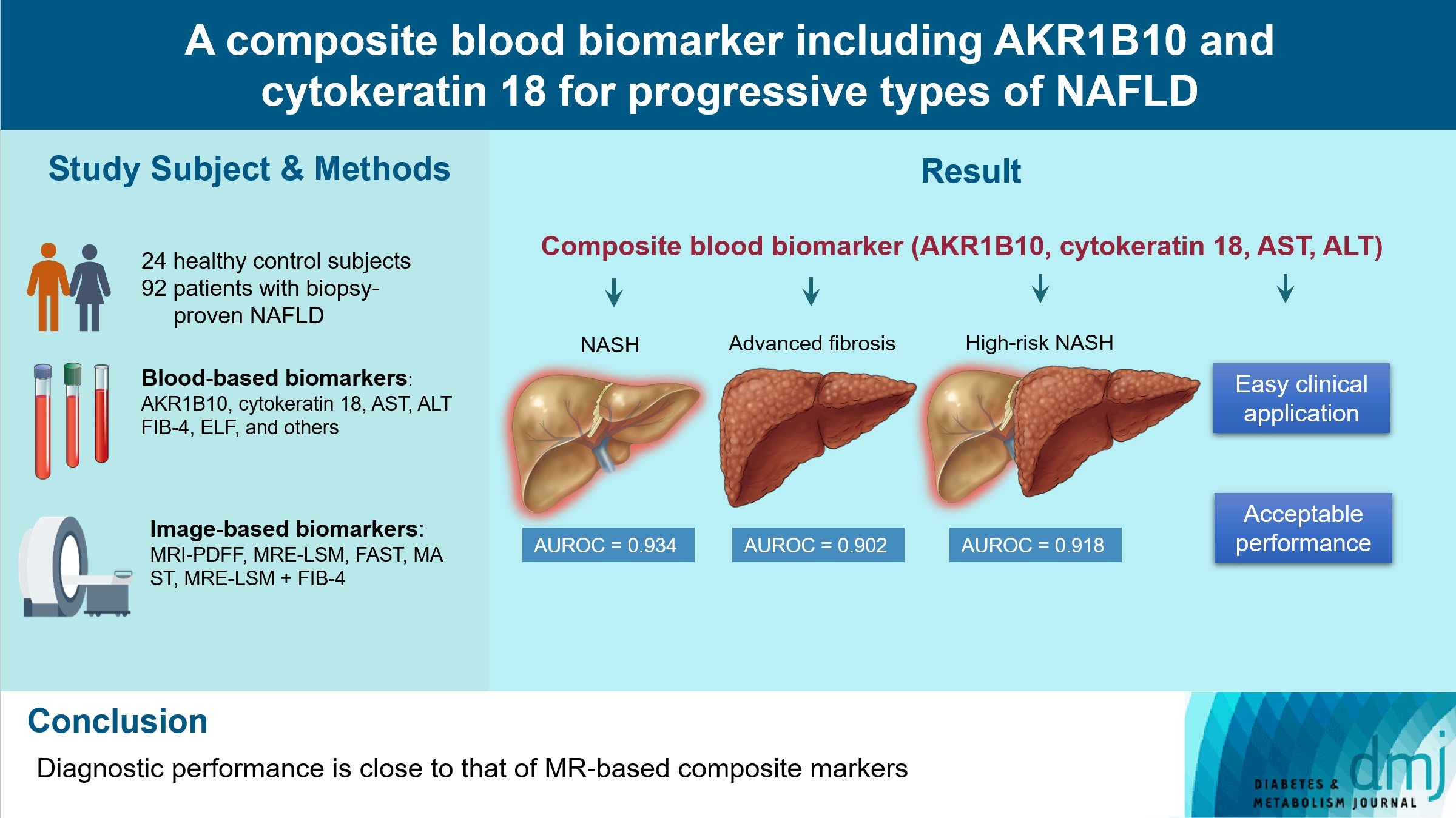
We aimed to evaluate whether composite blood biomarkers including aldo-keto reductase family 1 member B10 (AKR1B10) and cytokeratin 18 (CK-18; a nonalcoholic steatohepatitis [NASH] marker) have clinically applicable performance for the diagnosis of NASH, advanced liver fibrosis, and high-risk NASH (NASH+significant fibrosis).
Methods
A total of 116 subjects including healthy control subjects and patients with biopsy-proven nonalcoholic fatty liver disease (NAFLD) were analyzed to assess composite blood-based and imaging-based biomarkers either singly or in combination.
Results
A composite blood biomarker comprised of AKR1B10, CK-18, aspartate aminotransferase (AST), and alanine aminotransferase (ALT) showed excellent performance for the diagnosis of, NASH, advanced fibrosis, and high-risk NASH, with area under the receiver operating characteristic curve values of 0.934 (95% confidence interval [CI], 0.888 to 0.981), 0.902 (95% CI, 0.832 to 0.971), and 0.918 (95% CI, 0.862 to 0.974), respectively. However, the performance of this blood composite biomarker was inferior to that various magnetic resonance (MR)-based composite biomarkers, such as proton density fat fraction/MR elastography- liver stiffness measurement (MRE-LSM)/ALT/AST for NASH, MRE-LSM+fibrosis-4 index for advanced fibrosis, and the known MR imaging-AST (MAST) score for high-risk NASH.
Conclusion
Our blood composite biomarker can be useful to distinguish progressive forms of NAFLD as an initial noninvasive test when MR-based tools are not available.
- Drug/Regimen
- Comparative Efficacy of Rosuvastatin Monotherapy and Rosuvastatin/Ezetimibe Combination Therapy on Insulin Sensitivity and Vascular Inflammatory Response in Patients with Type 2 Diabetes Mellitus
- Ji Hye Han, Kyong Hye Joung, Jun Choul Lee, Ok Soon Kim, Sorim Choung, Ji Min Kim, Yea Eun Kang, Hyon-Seung Yi, Ju Hee Lee, Bon Jeong Ku, Hyun Jin Kim
- Diabetes Metab J. 2024;48(1):112-121. Published online January 3, 2024
- DOI: https://doi.org/10.4093/dmj.2022.0402
- 2,107 View
- 224 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
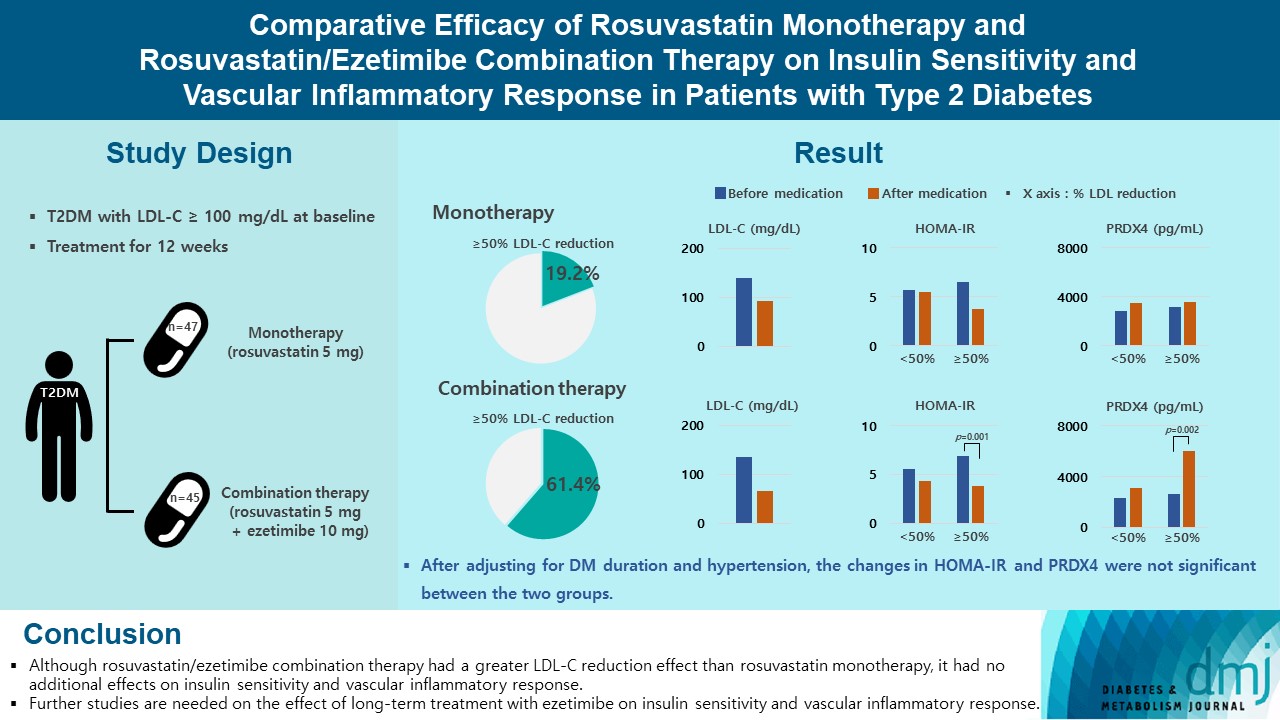
Type 2 diabetes mellitus (T2DM) induces endothelial dysfunction and inflammation, which are the main factors for atherosclerosis and cardiovascular disease. The present study aimed to compare the effects of rosuvastatin monotherapy and rosuvastatin/ezetimibe combination therapy on lipid profile, insulin sensitivity, and vascular inflammatory response in patients with T2DM.
Methods
A total of 101 patients with T2DM and dyslipidemia were randomized to either rosuvastatin monotherapy (5 mg/day, n=47) or rosuvastatin/ezetimibe combination therapy (5 mg/10 mg/day, n=45) and treated for 12 weeks. Serum lipids, glucose, insulin, soluble intercellular adhesion molecule-1 (sICAM-1), and peroxiredoxin 4 (PRDX4) levels were determined before and after 12 weeks of treatment.
Results
The reduction in low density lipoprotein cholesterol (LDL-C) by more than 50% from baseline after treatment was more in the combination therapy group. The serum sICAM-1 levels increased significantly in both groups, but there was no difference between the two groups. The significant changes in homeostasis model assessment of insulin resistance (HOMA-IR) and PRDX4 were confirmed only in the subgroup in which LDL-C was reduced by 50% or more in the combination therapy group. However, after adjusting for diabetes mellitus duration and hypertension, the changes in HOMA-IR and PRDX4 were not significant between the two groups.
Conclusion
Although rosuvastatin/ezetimibe combination therapy had a greater LDL-C reduction effect than rosuvastatin monotherapy, it had no additional effects on insulin sensitivity and vascular inflammatory response. Further studies are needed on the effect of long-term treatment with ezetimibe on insulin sensitivity and vascular inflammatory response. -
Citations
Citations to this article as recorded by- Combining Ezetimibe and Rosuvastatin: Impacts on Insulin Sensitivity and Vascular Inflammation in Patients with Type 2 Diabetes Mellitus
Eun Roh
Diabetes & Metabolism Journal.2024; 48(1): 55. CrossRef
- Combining Ezetimibe and Rosuvastatin: Impacts on Insulin Sensitivity and Vascular Inflammation in Patients with Type 2 Diabetes Mellitus
- Guideline/Fact Sheet
- 2023 Clinical Practice Guidelines for Diabetes Mellitus of the Korean Diabetes Association
- Jong Han Choi, Kyung Ae Lee, Joon Ho Moon, Suk Chon, Dae Jung Kim, Hyun Jin Kim, Nan Hee Kim, Ji A Seo, Mee Kyoung Kim, Jeong Hyun Lim, YoonJu Song, Ye Seul Yang, Jae Hyeon Kim, You-Bin Lee, Junghyun Noh, Kyu Yeon Hur, Jong Suk Park, Sang Youl Rhee, Hae Jin Kim, Hyun Min Kim, Jung Hae Ko, Nam Hoon Kim, Chong Hwa Kim, Jeeyun Ahn, Tae Jung Oh, Soo-Kyung Kim, Jaehyun Kim, Eugene Han, Sang-Man Jin, Won Suk Choi, Min Kyong Moon, Committee of Clinical Practice Guidelines, Korean Diabetes Association
- Diabetes Metab J. 2023;47(5):575-594. Published online September 26, 2023
- DOI: https://doi.org/10.4093/dmj.2023.0282
- 5,137 View
- 641 Download
- 8 Web of Science
- 14 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
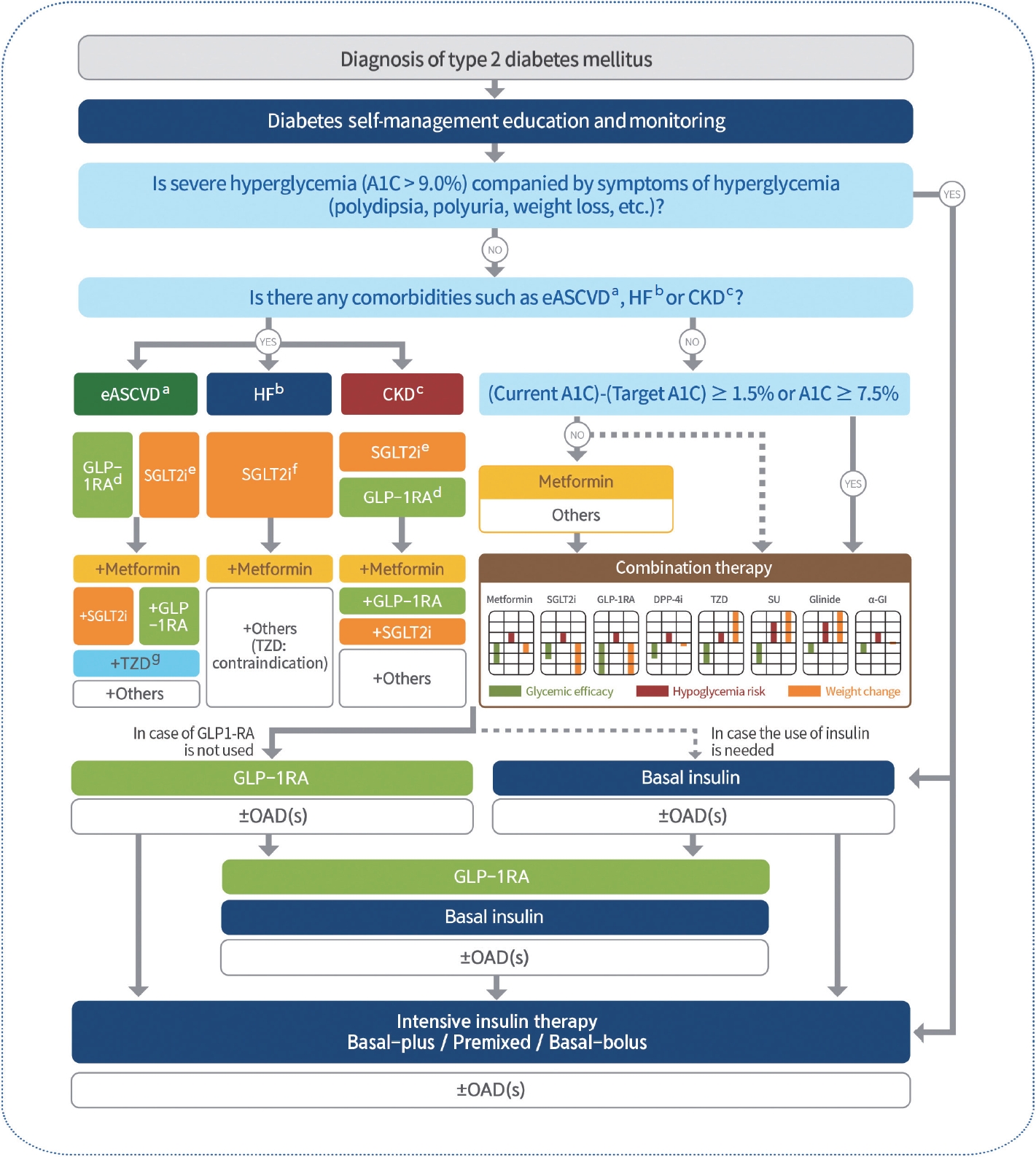
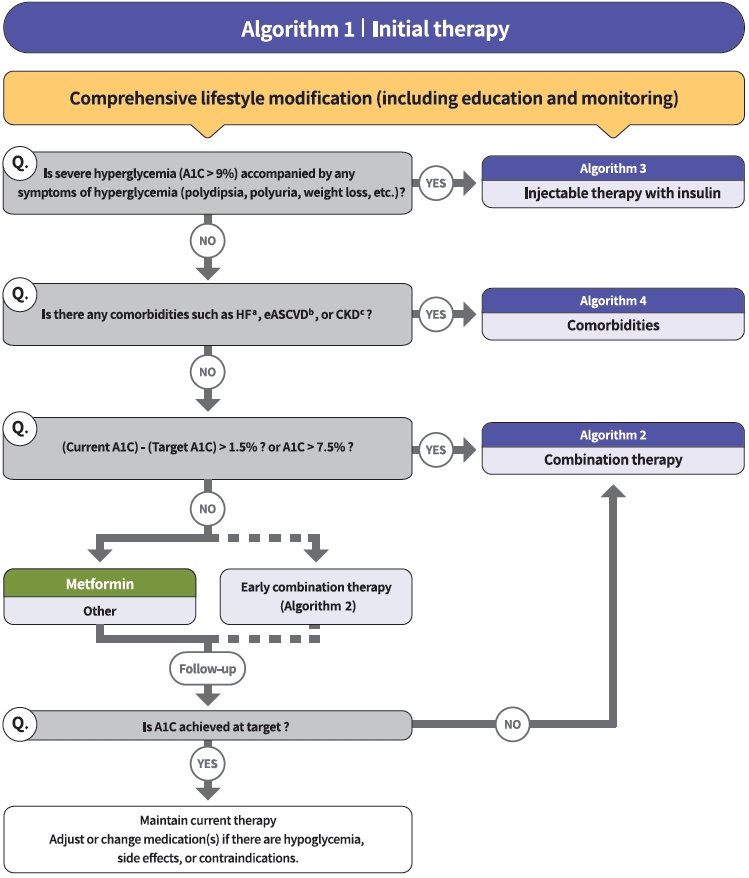
ePub - In May 2023, the Committee of Clinical Practice Guidelines of the Korean Diabetes Association published the revised clinical practice guidelines for Korean adults with diabetes and prediabetes. We incorporated the latest clinical research findings through a comprehensive systematic literature review and applied them in a manner suitable for the Korean population. These guidelines are designed for all healthcare providers nationwide, including physicians, diabetes experts, and certified diabetes educators who manage patients with diabetes or individuals at risk of developing diabetes. Based on recent changes in international guidelines and the results of a Korean epidemiological study, the recommended age for diabetes screening has been lowered. In collaboration with the relevant Korean medical societies, recently revised guidelines for managing hypertension and dyslipidemia in patients with diabetes have been incorporated into this guideline. An abridgment containing practical information on patient education and systematic management in the clinic was published separately.
-
Citations
Citations to this article as recorded by- Mortality in metabolic dysfunction-associated steatotic liver disease: A nationwide population-based cohort study
Eugene Han, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha, Sang Hoon Ahn, Yong-ho Lee, Seung Up Kim
Metabolism.2024; 152: 155789. CrossRef - Letter by In-Kyung Jeong Regarding Article, Trends in Prevalence of Hypertriglyceridemia and Related Factors in Korean Adults: A Serial Cross-Sectional Study
In-Kyung Jeong
Journal of Lipid and Atherosclerosis.2024; 13(1): 80. CrossRef - Association between cardiovascular disease risk and incident type 2 diabetes mellitus in individuals with prediabetes: A retrospective cohort study
Myung Jin Kim, Yun Kyung Cho, Chang Hee Jung, Woo Je Lee
Diabetes Research and Clinical Practice.2024; 208: 111125. CrossRef - Korea Hypertension Fact Sheet 2023: analysis of nationwide population-based data with a particular focus on hypertension in special populations
Hyeon Chang Kim, Hokyou Lee, Hyeok-Hee Lee, Dasom Son, Minsung Cho, Sojung Shin, Yeeun Seo, Eun-Jin kim, Song Vogue Ahn, Sun Ha Jee, Sungha Park, Hae-Young Lee, Min Ho Shin, Sang-Hyun Ihm, Seung Won Lee, Jong Ku Park, Il Suh, Tae-Yong Lee
Clinical Hypertension.2024;[Epub] CrossRef - Diabetes Duration, Cholesterol Levels, and Risk of Cardiovascular Diseases in Individuals With Type 2 Diabetes
Mee Kyoung Kim, Kyu Na Lee, Kyungdo Han, Seung-Hwan Lee
The Journal of Clinical Endocrinology & Metabolism.2024;[Epub] CrossRef - Effect of Adding Apolipoprotein B Testing on the Prevalence of Dyslipidemia and Risk of Cardiovascular Disease in the Korean Adult Population
Rihwa Choi, Sang Gon Lee, Eun Hee Lee
Metabolites.2024; 14(3): 169. CrossRef - A self-powered and supercapacitive microneedle continuous glucose monitoring system with a wide range of glucose detection capabilities
Hye-Jun Kil, Jang Hyeon Kim, Kanghae Lee, Tae-Uk Kang, Ju-Hyun Yoo, Yong-ho Lee, Jin-Woo Park
Biosensors and Bioelectronics.2024; 257: 116297. CrossRef - Cardiorenal outcomes and mortality after sodium‐glucose cotransporter‐2 inhibitor initiation in type 2 diabetes patients with percutaneous coronary intervention history
Jin Hwa Kim, Young Sang Lyu, BongSeong Kim, Mee Kyung Kim, Sang Yong Kim, Ki‐Hyun Baek, Ki‐Ho Song, Kyungdo Han, Hyuk‐Sang Kwon
Diabetes, Obesity and Metabolism.2024;[Epub] CrossRef - Management of Dyslipidemia in Patients with Diabetes Mellitus
Kyung Ae Lee
The Journal of Korean Diabetes.2023; 24(3): 111. CrossRef - 2023 Clinical Practice Guidelines for Diabetes: Recommendations for Pharmacological Treatment of Type 2 Diabetes
Junghyun Noh
The Journal of Korean Diabetes.2023; 24(3): 127. CrossRef - 2023 Clinical Practice Guidelines for Diabetes
Min Kyong Moon
The Journal of Korean Diabetes.2023; 24(3): 120. CrossRef - 2023 Clinical Practice Guidelines for Diabetes: Management of Cardiovascular Risk Factors
Ye Seul Yang
The Journal of Korean Diabetes.2023; 24(3): 135. CrossRef - A 33-Year-Old Man Presented with Abdominal Pain and Vomiting Starting a Day Ago
Jong Han Choi
The Korean Journal of Medicine.2023; 98(6): 289. CrossRef - Comorbidity Patterns and Management in Inpatients with Endocrine Diseases by Age Groups in South Korea: Nationwide Data
Sung-Soo Kim, Hun-Sung Kim
Journal of Personalized Medicine.2023; 14(1): 42. CrossRef
- Mortality in metabolic dysfunction-associated steatotic liver disease: A nationwide population-based cohort study
- Basic Research
- Pharmacologic Activation of Angiotensin-Converting Enzyme II Alleviates Diabetic Cardiomyopathy in db/db Mice by Reducing Reactive Oxidative Stress
- Donghyun Kim, Wooju Jeong, Yumin Kim, Jibeom Lee, Sung Woo Cho, Chang-Myung Oh, Raekil Park
- Diabetes Metab J. 2023;47(4):487-499. Published online April 25, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0125
- 2,299 View
- 150 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
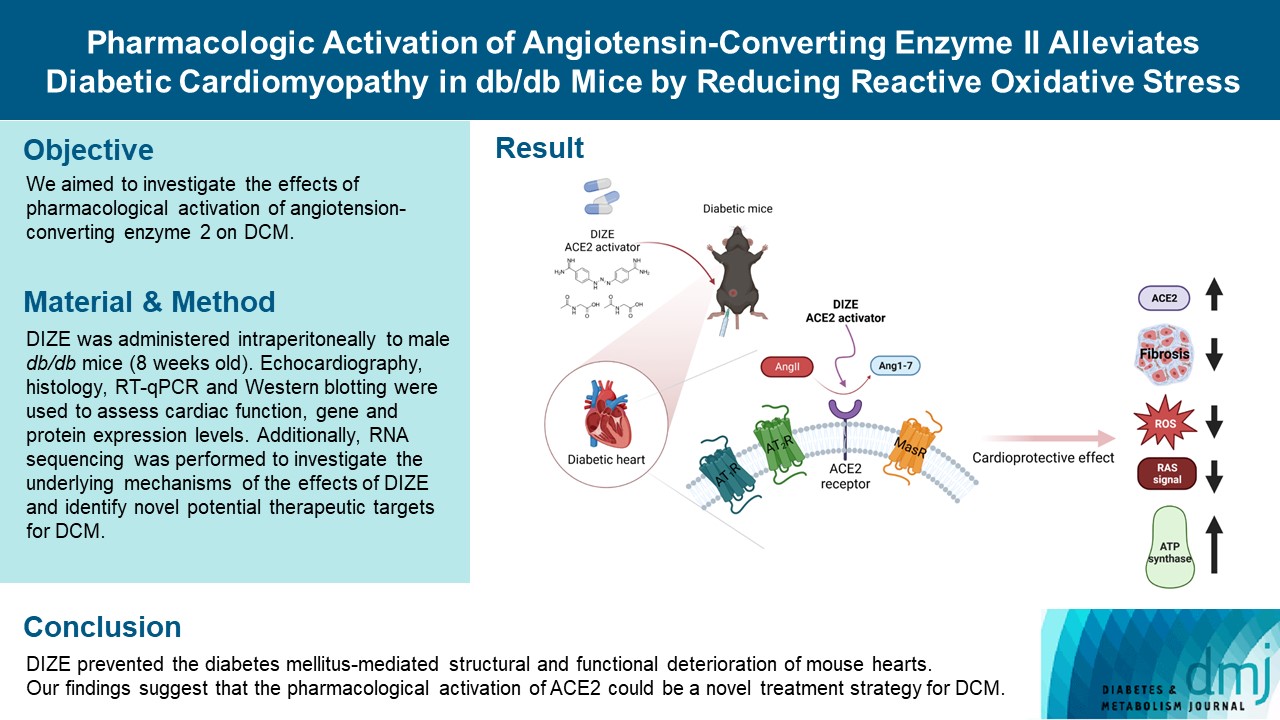
Diabetes mellitus is one of the most common chronic diseases worldwide, and cardiovascular disease is the leading cause of morbidity and mortality in diabetic patients. Diabetic cardiomyopathy (DCM) is a phenomenon characterized by a deterioration in cardiac function and structure, independent of vascular complications. Among many possible causes, the renin-angiotensin-aldosterone system and angiotensin II have been proposed as major drivers of DCM development. In the current study, we aimed to investigate the effects of pharmacological activation of angiotensin-converting enzyme 2 (ACE2) on DCM.
Methods
The ACE2 activator diminazene aceturate (DIZE) was administered intraperitoneally to male db/db mice (8 weeks old) for 8 weeks. Transthoracic echocardiography was used to assess cardiac mass and function in mice. Cardiac structure and fibrotic changes were examined using histology and immunohistochemistry. Gene and protein expression levels were examined using quantitative reverse transcription polymerase chain reaction and Western blotting, respectively. Additionally, RNA sequencing was performed to investigate the underlying mechanisms of the effects of DIZE and identify novel potential therapeutic targets for DCM.
Results
Echocardiography revealed that in DCM, the administration of DIZE significantly improved cardiac function as well as reduced cardiac hypertrophy and fibrosis. Transcriptome analysis revealed that DIZE treatment suppresses oxidative stress and several pathways related to cardiac hypertrophy.
Conclusion
DIZE prevented the diabetes mellitus-mediated structural and functional deterioration of mouse hearts. Our findings suggest that the pharmacological activation of ACE2 could be a novel treatment strategy for DCM.
- Guideline/Fact Sheet
- 2021 Clinical Practice Guidelines for Diabetes Mellitus in Korea
- Kyu Yeon Hur, Min Kyong Moon, Jong Suk Park, Soo-Kyung Kim, Seung-Hwan Lee, Jae-Seung Yun, Jong Ha Baek, Junghyun Noh, Byung-Wan Lee, Tae Jung Oh, Suk Chon, Ye Seul Yang, Jang Won Son, Jong Han Choi, Kee Ho Song, Nam Hoon Kim, Sang Yong Kim, Jin Wha Kim, Sang Youl Rhee, You-Bin Lee, Sang-Man Jin, Jae Hyeon Kim, Chong Hwa Kim, Dae Jung Kim, SungWan Chun, Eun-Jung Rhee, Hyun Min Kim, Hyun Jung Kim, Donghyun Jee, Jae Hyun Kim, Won Seok Choi, Eun-Young Lee, Kun-Ho Yoon, Seung-Hyun Ko, Committee of Clinical Practice Guidelines, Korean Diabetes Association
- Diabetes Metab J. 2021;45(4):461-481. Published online July 30, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0156
- 24,036 View
- 1,630 Download
- 122 Web of Science
- 141 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub 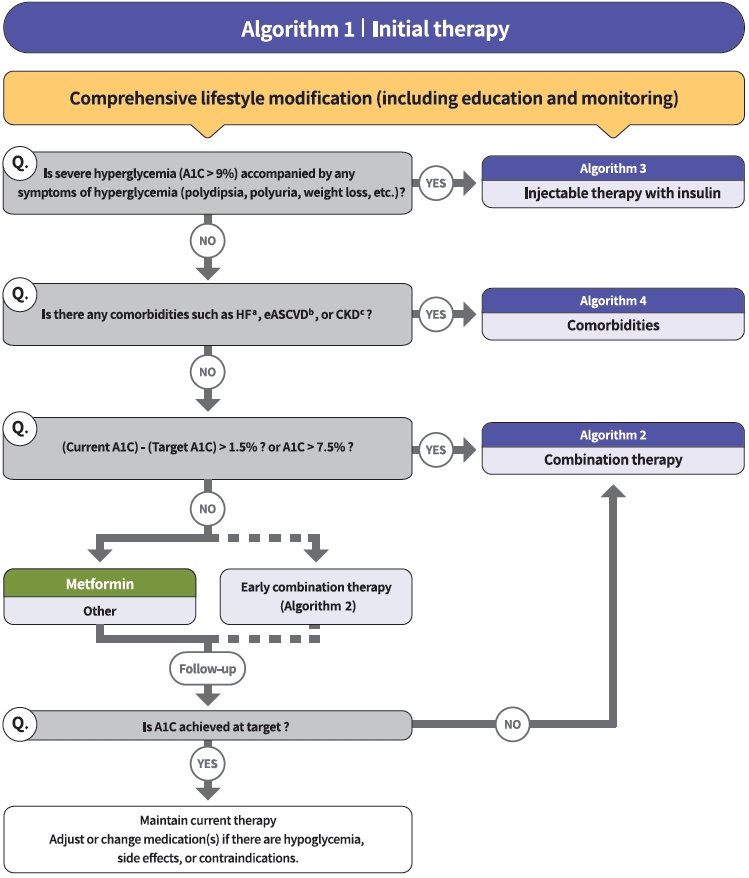
- The Committee of Clinical Practice Guidelines of the Korean Diabetes Association (KDA) updated the previous clinical practice guidelines for Korean adults with diabetes and prediabetes and published the seventh edition in May 2021. We performed a comprehensive systematic review of recent clinical trials and evidence that could be applicable in real-world practice and suitable for the Korean population. The guideline is provided for all healthcare providers including physicians, diabetes experts, and certified diabetes educators across the country who manage patients with diabetes or the individuals at the risk of developing diabetes mellitus. The recommendations for screening diabetes and glucose-lowering agents have been revised and updated. New sections for continuous glucose monitoring, insulin pump use, and non-alcoholic fatty liver disease in patients with diabetes mellitus have been added. The KDA recommends active vaccination for coronavirus disease 2019 in patients with diabetes during the pandemic. An abridgement that contains practical information for patient education and systematic management in the clinic was published separately.
-
Citations
Citations to this article as recorded by- Impact of Subclinical Atrial Function on the Prognosis of Patients With Atrial Fibrillation and Metabolic Syndrome
Hyun-Jin Kim
CardioMetabolic Syndrome Journal.2024; 4(1): 36. CrossRef - Associations of omega-3 fatty acids vs. fenofibrate with adverse cardiovascular outcomes in people with metabolic syndrome: propensity matched cohort study
Nam Hoon Kim, Ji Yoon Kim, Jimi Choi, Sin Gon Kim
European Heart Journal - Cardiovascular Pharmacotherapy.2024; 10(2): 118. CrossRef - A Multicenter, Randomized, Open-Label Study to Compare the Effects of Gemigliptin Add-on or Escalation of Metformin Dose on Glycemic Control and Safety in Patients with Inadequately Controlled Type 2 Diabetes Mellitus Treated with Metformin and SGLT-2 Inh
Hae Jin Kim, Jung Hyun Noh, Min Kyong Moon, Sung Hee Choi, Seung-Hyun Ko, Eun-Jung Rhee, Kyu Yeon Hur, In-Kyung Jeong, Mark Yorek
Journal of Diabetes Research.2024; 2024: 1. CrossRef - Efficacy and Safety of Once-Weekly Semaglutide Versus Once-Daily Sitagliptin as Metformin Add-on in a Korean Population with Type 2 Diabetes
Byung-Wan Lee, Young Min Cho, Sin Gon Kim, Seung-Hyun Ko, Soo Lim, Amine Dahaoui, Jin Sook Jeong, Hyo Jin Lim, Jae Myung Yu
Diabetes Therapy.2024; 15(2): 547. CrossRef - Real-World Continuous Glucose Monitoring Data from a Population with Type 1 Diabetes in South Korea: Nationwide Single-System Analysis
Ji Yoon Kim, Sang-Man Jin, Sarah B. Andrade, Boyang Chen, Jae Hyeon Kim
Diabetes Technology & Therapeutics.2024;[Epub] CrossRef - Association between Dyslipidemia and Glycated Hemoglobin in a Population-Based Study
Purum Kang, Ka Young Kim, Hye Young Shin
Metabolites.2024; 14(2): 92. CrossRef - Outcomes of Various Classes of Oral Antidiabetic Drugs on Nonalcoholic Fatty Liver Disease
Heejoon Jang, Yeonjin Kim, Dong Hyeon Lee, Sae Kyung Joo, Bo Kyung Koo, Soo Lim, Woojoo Lee, Won Kim
JAMA Internal Medicine.2024; 184(4): 375. CrossRef - View on Metformin: Antidiabetic and Pleiotropic Effects, Pharmacokinetics, Side Effects, and Sex-Related Differences
Guglielmina Froldi
Pharmaceuticals.2024; 17(4): 478. CrossRef - Comparison between a tubeless, on-body automated insulin delivery system and a tubeless, on-body sensor-augmented pump in type 1 diabetes: a multicentre randomised controlled trial
Ji Yoon Kim, Sang-Man Jin, Eun Seok Kang, Soo Heon Kwak, Yeoree Yang, Jee Hee Yoo, Jae Hyun Bae, Jun Sung Moon, Chang Hee Jung, Ji Cheol Bae, Sunghwan Suh, Sun Joon Moon, Sun Ok Song, Suk Chon, Jae Hyeon Kim
Diabetologia.2024;[Epub] CrossRef - Inhibition of sodium-glucose cotransporter-2 and liver-related complications in individuals with diabetes: a Mendelian randomization and population-based cohort study
Sung Won Chung, Hye-Sung Moon, Hyunjae Shin, Hyein Han, Sehoon Park, Heejin Cho, Jeayeon Park, Moon Haeng Hur, Min Kyung Park, Sung-Ho Won, Yun Bin Lee, Eun Ju Cho, Su Jong Yu, Dong Ki Kim, Jung-Hwan Yoon, Jeong-Hoon Lee, Yoon Jun Kim
Hepatology.2024;[Epub] CrossRef - Efficacy of intermittent short‐term use of a real‐time continuous glucose monitoring system in non‐insulin–treated patients with type 2 diabetes: A randomized controlled trial
Sun Joon Moon, Kyung‐Soo Kim, Woo Je Lee, Mi Yeon Lee, Robert Vigersky, Cheol‐Young Park
Diabetes, Obesity and Metabolism.2023; 25(1): 110. CrossRef - Therapeutic Effects of Switching to Anagliptin from Other DPP-4 Inhibitors in T2DM Patients with Inadequate Glycemic Control: A Non-interventional, Single-Arm, Open-Label, Multicenter Observational Study
Sang-Yong Kim, Sungrae Kim
Diabetes Therapy.2023; 14(1): 109. CrossRef - Low Skeletal Muscle Mass Accompanied by Abdominal Obesity Additively Increases the Risk of Incident Type 2 Diabetes
Ji Eun Jun, Seung-Eun Lee, You-Bin Lee, Gyuri Kim, Sang-Man Jin, Jae Hwan Jee, Jae Hyeon Kim
The Journal of Clinical Endocrinology & Metabolism.2023; 108(5): 1173. CrossRef - Diabetes screening in South Korea: a new estimate of the number needed to screen to detect diabetes
Kyoung Hwa Ha, Kyung Ae Lee, Kyung-Do Han, Min Kyong Moon, Dae Jung Kim
The Korean Journal of Internal Medicine.2023; 38(1): 93. CrossRef - Justicia carnea extracts ameliorated hepatocellular damage in streptozotocin-induced type 1 diabetic male rats via decrease in oxidative stress, inflammation and increasing other risk markers
John Adeolu Falode, Oluwaseun Igbekele Ajayi, Tolulope Victoria Isinkaye, Akinwunmi Oluwaseun Adeoye, Basiru Olaitan Ajiboye, Bartholomew I. C. Brai
Biomarkers.2023; 28(2): 177. CrossRef - Sex differences in the impact of diabetes mellitus on tuberculosis recurrence: a retrospective national cohort study
Dararat Eksombatchai, Dawoon Jeong, Jeongha Mok, Doosoo Jeon, Hee-Yeon Kang, Hee Jin Kim, Hee-Sun Kim, Hongjo Choi, Young Ae Kang
International Journal of Infectious Diseases.2023; 127: 1. CrossRef - The Predictive Ability of C-Peptide in Distinguishing Type 1 Diabetes From Type 2 Diabetes: A Systematic Review and Meta-Analysis
Sajid Iqbal, Abdulrahim Abu Jayyab, Ayah Mohammad Alrashdi, Silvia Reverté-Villarroya
Endocrine Practice.2023; 29(5): 379. CrossRef - Anagliptin twice‐daily regimen improves glycaemic variability in subjects with type 2 diabetes: A double‐blind, randomized controlled trial
Yong‐ho Lee, Doo‐Man Kim, Jae Myung Yu, Kyung Mook Choi, Sin Gon Kim, Kang Seo Park, Hyun‐Shik Son, Choon Hee Chung, Kyu Jeung Ahn, Soon Hee Lee, Ki‐Ho Song, Su Kyoung Kwon, Hyeong Kyu Park, Kyu Chang Won, Hak Chul Jang
Diabetes, Obesity and Metabolism.2023; 25(5): 1174. CrossRef - Implementation of five machine learning methods to predict the 52-week blood glucose level in patients with type 2 diabetes
Xiaomin Fu, Yuhan Wang, Ryan S. Cates, Nan Li, Jing Liu, Dianshan Ke, Jinghua Liu, Hongzhou Liu, Shuangtong Yan
Frontiers in Endocrinology.2023;[Epub] CrossRef - Lipid Management in Korean People With Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
Ye Seul Yang, Hack-Lyoung Kim, Sang-Hyun Kim, Min Kyong Moon
Journal of Lipid and Atherosclerosis.2023; 12(1): 12. CrossRef - The Efficacy of Treatment Intensification by Quadruple Oral Therapy Compared to GLP-1RA Therapy in Poorly Controlled Type 2 Diabetes Mellitus Patients: A Real-world Data Study
Minyoung Kim, Hosu Kim, Kyong Young Kim, Soo Kyoung Kim, Junghwa Jung, Jong Ryeal Hahm, Jaehoon Jung, Jong Ha Baek
Diabetes & Metabolism Journal.2023; 47(1): 135. CrossRef - Safety and Effectiveness of Empagliflozin in Korean Patients with Type 2 Diabetes Mellitus: Results from a Nationwide Post-Marketing Surveillance
Jun Sung Moon, Nam Hoon Kim, Jin Oh Na, Jae Hyoung Cho, In-Kyung Jeong, Soon Hee Lee, Ji-Oh Mok, Nan Hee Kim, Dong Jin Chung, Jinhong Cho, Dong Woo Lee, Sun Woo Lee, Kyu Chang Won
Diabetes & Metabolism Journal.2023; 47(1): 82. CrossRef - Evaluation and Management of Patients With Diabetes and Heart Failure: A Korean Diabetes Association and Korean Society of Heart Failure Consensus Statement
Kyu-Sun Lee, Junghyun Noh, Seong-Mi Park, Kyung Mook Choi, Seok-Min Kang, Kyu-Chang Won, Hyun-Jai Cho, Min Kyong Moon
International Journal of Heart Failure.2023; 5(1): 1. CrossRef - Influenza vaccination trend and related factors among patients with diabetes in Korea: Analysis using a nationwide database
Dong-Hwa Lee, Bumhee Yang, Seonhye Gu, Eung-Gook Kim, Youlim Kim, Hyung Koo Kang, Yeong Hun Choe, Hyun Jeong Jeon, Seungyong Park, Hyun Lee
Frontiers in Endocrinology.2023;[Epub] CrossRef - Optimal Low-Density Lipoprotein Cholesterol Level for Primary Prevention in Koreans with Type 2 Diabetes Mellitus
Ji Yoon Kim, Nam Hoon Kim
Diabetes & Metabolism Journal.2023; 47(1): 42. CrossRef - Evaluation and Management of Patients with Diabetes and Heart Failure: A Korean Diabetes Association and Korean Society of Heart Failure Consensus Statement
Kyu-Sun Lee, Junghyun Noh, Seong-Mi Park, Kyung Mook Choi, Seok-Min Kang, Kyu-Chang Won, Hyun-Jai Cho, Min Kyong Moon
Diabetes & Metabolism Journal.2023; 47(1): 10. CrossRef - Lipid Management in Korean People with Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
Ye Seul Yang, Hack-Lyoung Kim, Sang-Hyun Kim, Min Kyong Moon
Diabetes & Metabolism Journal.2023; 47(1): 1. CrossRef - Association between Low-Density Lipoprotein Cholesterol Level and Cardiovascular Outcomes in Korean Adults: A Nationwide Cohort Study
Junghyun Noh, Min Kyong Moon, Eun-Jung Rhee, Sang Hyun Park, Hyeon Chang Kim, Byung Jin Kim, Hae Jin Kim, Seonghoon Choi, Jin Oh Na, Young Youl Hyun, Bum Joon Kim, Kyung-Do Han, In-Kyung Jeong
Diabetes & Metabolism Journal.2023; 47(1): 59. CrossRef - Analysis of the Incidence of Type 2 Diabetes, Requirement of Insulin Treatment, and Diabetes-Related Complications among Patients with Cancer
Su Jung Lee, Chulho Kim, Hyunjae Yu, Dong-Kyu Kim
Cancers.2023; 15(4): 1094. CrossRef - The 2022 focused update of the 2018 Korean Hypertension Society Guidelines for the management of hypertension
Hack-Lyoung Kim, Eun Mi Lee, Shin Young Ahn, Kwang-il Kim, Hyeon Chang Kim, Ju Han Kim, Hae-Young Lee, Jang Hoon Lee, Jong-Moo Park, Eun Joo Cho, Sungha Park, Jinho Shin, Young-Kwon Kim
Clinical Hypertension.2023;[Epub] CrossRef - Consistency of 1-day and 3-day average dietary intake and the relationship of dietary intake with blood glucose, hbA1c, BMI, and lipids in patients with type 2 diabetes
DaeEun Lee, Haejung Lee, Sangeun Lee, MinJin Lee, Ah Reum Khang
Journal of Korean Biological Nursing Science.2023; 25(1): 20. CrossRef - Efficacy and safety of enavogliflozin versus dapagliflozin added to metformin plus gemigliptin treatment in patients with type 2 diabetes: A double-blind, randomized, comparator-active study: ENHANCE-D study
Kyung-Soo Kim, Kyung Ah Han, Tae Nyun Kim, Cheol-Young Park, Jung Hwan Park, Sang Yong Kim, Yong Hyun Kim, Kee Ho Song, Eun Seok Kang, Chul Sik Kim, Gwanpyo Koh, Jun Goo Kang, Mi Kyung Kim, Ji Min Han, Nan Hee Kim, Ji Oh Mok, Jae Hyuk Lee, Soo Lim, Sang S
Diabetes & Metabolism.2023; 49(4): 101440. CrossRef - Effect of olmesartan and amlodipine on serum angiotensin-(1–7) levels and kidney and vascular function in patients with type 2 diabetes and hypertension
Kyuho Kim, Ji Hye Moon, Chang Ho Ahn, Soo Lim
Diabetology & Metabolic Syndrome.2023;[Epub] CrossRef - Menopausal hormone therapy and the risk of type 2 diabetes mellitus: Health Insurance Database in South Korea–based retrospective cohort study
Jin-Sung Yuk, Jung Min Kim
Menopause.2023; 30(5): 497. CrossRef - Intensified Multifactorial Intervention in Patients with Type 2 Diabetes Mellitus
Takayoshi Sasako, Toshimasa Yamauchi, Kohjiro Ueki
Diabetes & Metabolism Journal.2023; 47(2): 185. CrossRef - Association between antidiabetic drugs and the incidence of atrial fibrillation in patients with type 2 diabetes: A nationwide cohort study in South Korea
Sunyoung Kim, So Young Park, Bongseong Kim, Chanyang Min, Wonyoung Cho, Dong Keon Yon, Joo Young Kim, Kyung-Do Han, Eun-Jung Rhee, Won-Young Lee, Sang Youl Rhee
Diabetes Research and Clinical Practice.2023; 198: 110626. CrossRef - Totally robotic Roux-en-Y gastric bypass in a morbidly obese patient in Korea: a case report
Ji Won Seo, Kyong-Hwa Jun
Journal of Minimally Invasive Surgery.2023; 26(1): 40. CrossRef - Effect of diabetes-specific oral nutritional supplements with allulose on weight and glycemic profiles in overweight or obese type 2 diabetic patients
Jihye Tak, Minkyung Bok, Hyunkyung Rho, Ju Hyun Park, Yunsook Lim, Suk Chon, Hyunjung Lim
Nutrition Research and Practice.2023; 17(2): 241. CrossRef - Associations Between Modifiable Risk Factors and Changes in Glycemic Status Among Individuals With Prediabetes
Salma Nabila, Ji-Eun Kim, Jaesung Choi, JooYong Park, Aesun Shin, Sang-Ah Lee, Jong-koo Lee, Daehee Kang, Ji-Yeob Choi
Diabetes Care.2023; 46(3): 535. CrossRef - Efficacy and safety of enavogliflozin, a novel SGLT2 inhibitor, in Korean people with type 2 diabetes: A 24‐week, multicentre, randomized, double‐blind, placebo‐controlled, phase III trial
Soo Heon Kwak, Kyung Ah Han, Kyung‐Soo Kim, Jae Myung Yu, EunSook Kim, Jong Chul Won, Jun Goo Kang, Choon Hee Chung, Seungjoon Oh, Sung Hee Choi, Kyu Chang Won, Sin Gon Kim, Seung Ah Cho, Bo Young Cho, Kyong Soo Park
Diabetes, Obesity and Metabolism.2023; 25(7): 1865. CrossRef - Adjusting the Use of Glucose-Lowering Agents in the Real-World Clinical Management of People with Type 2 Diabetes: A Narrative Review
Siew Pheng Chan, Lee-Ling Lim, Juliana C. N. Chan, David R. Matthews
Diabetes Therapy.2023; 14(5): 823. CrossRef - The association of perfluoroalkyl substances (PFAS) exposure and kidney function in Korean adolescents using data from Korean National Environmental Health Survey (KoNEHS) cycle 4 (2018–2020): a cross-sectional study
Jisuk Yun, Eun-Chul Jang, Soon-Chan Kwon, Young-Sun Min, Yong-Jin Lee
Annals of Occupational and Environmental Medicine.2023;[Epub] CrossRef - A Comparison of the Pharmacokinetics and Safety of Dapagliflozin Formate, an Ester Prodrug of Dapagliflozin, to Dapagliflozin Propanediol Monohydrate in Healthy Subjects
Hyun Chul Kim, Sangmi Lee, Siyoung Sung, Eunjin Kim, In-Jin Jang, Jae-Yong Chung
Drug Design, Development and Therapy.2023; Volume 17: 1203. CrossRef - Efficacy and safety of monotherapy with enavogliflozin in Korean patients with type 2 diabetes mellitus: Results of a 12‐week, multicentre, randomized, double‐blind, placebo‐controlled, phase 2 trial
Ye Seul Yang, Kyung Wan Min, Seok‐O Park, Kyung‐Soo Kim, Jae Myung Yu, Eun‐Gyoung Hong, Sung Rae Cho, Kyu Chang Won, Yong Hyun Kim, Seungjoon Oh, Sung Hee Choi, Gwanpyo Koh, Wan Huh, Su Young Kim, Kyong Soo Park
Diabetes, Obesity and Metabolism.2023; 25(8): 2096. CrossRef - An Integrated Digital Health Care Platform for Diabetes Management With AI-Based Dietary Management: 48-Week Results From a Randomized Controlled Trial
You-Bin Lee, Gyuri Kim, Ji Eun Jun, Hyunjin Park, Woo Je Lee, You-Cheol Hwang, Jae Hyeon Kim
Diabetes Care.2023; 46(5): 959. CrossRef - Performance of Simple Fibrosis Score in Non-Alcoholic Fatty Liver Disease with and without Type 2 Diabetes
Seung Min Chung, Min Kyu Kang, Jun Sung Moon, Jung Gil Park
Endocrinology and Metabolism.2023; 38(2): 277. CrossRef - Correlation analysis of cancer incidence after pravastatin treatment
Jin Yu, Raeun Kim, Jiwon Shinn, Man Young Park, Hun-Sung Kim
Cardiovascular Prevention and Pharmacotherapy.2023; 5(2): 61. CrossRef - Comparison of the effects of gemigliptin versus glimepiride on cardiac function in patients with type 2 diabetes uncontrolled with metformin: The gemi‐heart study
Seung Min Chung, Jun Sung Moon, Jun Hwa Hong, In‐Chang Hwang, Soo Lim
Diabetes, Obesity and Metabolism.2023; 25(8): 2181. CrossRef - The era of continuous glucose monitoring and its expanded role in type 2 diabetes
Jin Yu, Jae‐Hyoung Cho, Seung‐Hwan Lee
Journal of Diabetes Investigation.2023; 14(7): 841. CrossRef - Impact of continuous glucose monitoring on glycemic control and its derived metrics in type 1 diabetes: a longitudinal study
So Hyun Cho, Seohyun Kim, You-Bin Lee, Sang-Man Jin, Kyu Yeon Hur, Gyuri Kim, Jae Hyeon Kim
Frontiers in Endocrinology.2023;[Epub] CrossRef - Impact of mental disorders on the risk of heart failure among Korean patients with diabetes: a cohort study
Tae Kyung Yoo, Kyung-Do Han, Eun-Jung Rhee, Won-Young Lee
Cardiovascular Diabetology.2023;[Epub] CrossRef - Asia-Pacific consensus recommendations for application of continuous glucose monitoring in diabetes management
Alice P.S. Kong, Soo Lim, Seung-Hyun Yoo, Linong Ji, Liming Chen, Yuqian Bao, Ester Yeoh, Siew-Pheng Chan, Chih-Yuan Wang, Viswanathan Mohan, Neale Cohen, Margaret J. McGill, Stephen M. Twigg
Diabetes Research and Clinical Practice.2023; 201: 110718. CrossRef - Chronic disease management program applied to type 2 diabetes patients and prevention of diabetic complications: a retrospective cohort study using nationwide data
Min Kyung Hyun, Jang Won Lee, Seung-Hyun Ko
BMC Public Health.2023;[Epub] CrossRef - Fatty Liver & Diabetes Statistics in Korea: Nationwide Data 2009 to 2017
Eugene Han, Kyung-Do Han, Yong-ho Lee, Kyung-Soo Kim, Sangmo Hong, Jung Hwan Park, Cheol-Young Park
Diabetes & Metabolism Journal.2023; 47(3): 347. CrossRef - Opening the Precision Diabetes Care through Digital Healthcare
Joonyub Lee, Jin Yu, Kun-Ho Yoon
Diabetes & Metabolism Journal.2023; 47(3): 307. CrossRef - Glycemia according to the Use of Continuous Glucose Monitoring among Adults with Type 1 Diabetes Mellitus in Korea: A Real-World Study
You-Bin Lee, Minjee Kim, Jae Hyeon Kim
Diabetes & Metabolism Journal.2023; 47(3): 405. CrossRef - Navigating the Seas of Glycemic Control: The Role of Continuous Glucose Monitoring in Type 1 Diabetes Mellitus
Jun Sung Moon
Diabetes & Metabolism Journal.2023; 47(3): 345. CrossRef - Lost in translation: assessing the nomenclature change for diabetic kidney disease in Japan
Tetsuya Babazono, Tatsumi Moriya
Diabetology International.2023; 14(4): 319. CrossRef - Effects of dapagliflozin compared with glimepiride on body composition in Asian patients with type 2 diabetes inadequately controlled with metformin: The BEYOND study
Hyeong Kyu Park, Kyoung‐Ah Kim, Kyung‐Wan Min, Tae‐Seo Sohn, In Kyung Jeong, Chul Woo Ahn, Nan‐Hee Kim, Ie Byung Park, Ho Chan Cho, Choon Hee Chung, Sung Hee Choi, Kang Seo Park, Seoung‐Oh Yang, Kwan Woo Lee
Diabetes, Obesity and Metabolism.2023; 25(9): 2743. CrossRef - Topic Modeling Analysis of Diabetes-Related Health Information during the Coronavirus Disease Pandemic
Soyoon Min, Jeongwon Han
Healthcare.2023; 11(13): 1871. CrossRef - Screening Test for Evaluation of Cardiovascular Disease in Patients with Diabetes
Ji-Oh Mok, Chan-Hee Jung
The Journal of Korean Diabetes.2023; 24(2): 76. CrossRef - Paradigm Shift in Management of Hyperglycemia in Patients with Type 2 Diabetes: Glucocentric versus Organ Protection
Jong Chul Won
The Journal of Korean Diabetes.2023; 24(2): 59. CrossRef - Association between type 2 diabetes mellitus and depression among Korean midlife women: a cross-sectional analysis study
You Lee Yang, Eun-Ok Im, Yunmi Kim
BMC Nursing.2023;[Epub] CrossRef - Fibrotic Burden in the Liver Differs Across Metabolic Dysfunction-Associated Fatty Liver Disease Subtypes
Tae Seop Lim, Ho Soo Chun, Soon Sun Kim, Ja Kyung Kim, Minjong Lee, Hyo Jung Cho, Seung Up Kim, Jae Youn Cheong
Gut and Liver.2023; 17(4): 610. CrossRef - Association between the number of pregnancies and cardiac target organ damages: a cross-sectional analysis of data from the Korean women’s chest pain registry (KoROSE)
Hack-Lyoung Kim, Hyun-Jin Kim, Mina Kim, Sang Min Park, Hyun Ju Yoon, Young Sup Byun, Seong-Mi Park, Mi-Seung Shin, Kyung-Soon Hong, Myung-A Kim
BMC Women's Health.2023;[Epub] CrossRef - Exercise therapy for diabetes mellitus
Chaiho Jeong, Tae-Seo Sohn
Journal of the Korean Medical Association.2023; 66(7): 427. CrossRef - Medical nutrition therapy for diabetes mellitus
Suk Chon
Journal of the Korean Medical Association.2023; 66(7): 421. CrossRef - Identification of individuals at risk of hepatocellular carcinoma: screening for clinically significant liver fibrosis in patients with T2DM
Tina Reinson, Ryan M Buchanan, Christopher D Byrne
Expert Review of Endocrinology & Metabolism.2023; 18(5): 355. CrossRef - Additive impact of diabetes and sarcopenia on all-cause and cardiovascular mortality: A longitudinal nationwide population-based study
Eyun Song, Soon Young Hwang, Min Jeong Park, Ahreum Jang, Kyeong Jin Kim, Ji Hee Yu, Nam Hoon Kim, Hye Jin Yoo, Ji A. Seo, Sin Gon Kim, Nan Hee Kim, Sei Hyun Baik, Kyung Mook Choi
Metabolism.2023; 148: 155678. CrossRef - Exposure to perfluoroalkyl and polyfluoroalkyl substances and risk of stroke in adults: a meta-analysis
Min Cheol Chang, Seung Min Chung, Sang Gyu Kwak
Reviews on Environmental Health.2023;[Epub] CrossRef - Risk of Pancreatic Cancer and Use of Dipeptidyl Peptidase 4 Inhibitors in Patients with Type 2 Diabetes: A Propensity Score-Matching Analysis
Mee Kyoung Kim, Kyungdo Han, Hyuk-Sang Kwon, Soon Jib Yoo
Endocrinology and Metabolism.2023; 38(4): 426. CrossRef - Incident infection risks depending on oral antidiabetic exposure in insulin-treated type 2 diabetes patients
Sanghwa Park, Jiseon Jeong, Yunna Woo, Yeo Jin Choi, Sooyoung Shin
Scientific Reports.2023;[Epub] CrossRef - Dyslipidemia Fact Sheet in South Korea, 2022
Eun-Sun Jin, Jee-Seon Shim, Sung Eun Kim, Jae Hyun Bae, Shinae Kang, Jong Chul Won, Min-Jeong Shin, Heung Yong Jin, Jenny Moon, Hokyou Lee, Hyeon Chang Kim, In-Kyung Jeong
Journal of Lipid and Atherosclerosis.2023; 12(3): 237. CrossRef - Diabetes Mellitus in the Elderly Adults in Korea: Based on Data from the Korea National Health and Nutrition Examination Survey 2019 to 2020
Seung-Hyun Ko, Kyung Do Han, Yong-Moon Park, Jae-Seung Yun, Kyuho Kim, Jae-Hyun Bae, Hyuk-Sang Kwon, Nan-Hee Kim
Diabetes & Metabolism Journal.2023; 47(5): 643. CrossRef - Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD): A State-of-the-Art Review
Wah-Kheong Chan, Kee-Huat Chuah, Ruveena Bhavani Rajaram, Lee-Ling Lim, Jeyakantha Ratnasingam, Shireene Ratna Vethakkan
Journal of Obesity & Metabolic Syndrome.2023; 32(3): 197. CrossRef - Management of Dyslipidemia in Patients with Diabetes Mellitus
Kyung Ae Lee
The Journal of Korean Diabetes.2023; 24(3): 111. CrossRef - 2023 Clinical Practice Guidelines for Diabetes: Management of Cardiovascular Risk Factors
Ye Seul Yang
The Journal of Korean Diabetes.2023; 24(3): 135. CrossRef - Dyslipidemia Fact Sheet in South Korea, 2022
Eun-Sun Jin, Jee-Seon Shim, Sung Eun Kim, Jae Hyun Bae, Shinae Kang, Jong Chul Won, Min-Jeong Shin, Heung Yong Jin, Jenny Moon, Hokyou Lee, Hyeon Chang Kim, In-Kyung Jeong
Diabetes & Metabolism Journal.2023; 47(5): 632. CrossRef - 2023 Clinical Practice Guidelines for Diabetes Mellitus of the Korean Diabetes Association
Jong Han Choi, Kyung Ae Lee, Joon Ho Moon, Suk Chon, Dae Jung Kim, Hyun Jin Kim, Nan Hee Kim, Ji A Seo, Mee Kyoung Kim, Jeong Hyun Lim, YoonJu Song, Ye Seul Yang, Jae Hyeon Kim, You-Bin Lee, Junghyun Noh, Kyu Yeon Hur, Jong Suk Park, Sang Youl Rhee, Hae J
Diabetes & Metabolism Journal.2023; 47(5): 575. CrossRef - Riesgo residual. Conclusiones
Ángel Cequier, José Luis Zamorano
Revista Española de Cardiología Suplementos.2023; 23: 25. CrossRef - Intake of Fruit and Glycemic Control in Korean Patients with Diabetes Mellitus Using the Korea National Health and Nutrition Examination Survey
Eunju Yoon, Ji Cheol Bae, Sunghwan Suh
Endocrinology and Metabolism.2023; 38(5): 538. CrossRef - 2023 Clinical Practice Guidelines for Diabetes
Min Kyong Moon
The Journal of Korean Diabetes.2023; 24(3): 120. CrossRef - Cumulative effect of impaired fasting glucose on the risk of dementia in middle-aged and elderly people: a nationwide cohort study
Jin Yu, Kyu-Na Lee, Hun-Sung Kim, Kyungdo Han, Seung-Hwan Lee
Scientific Reports.2023;[Epub] CrossRef - Coleus forskohlii Root Extract (ForcslimTM) as a Prospective Antidiabetic Agent: In vitro Glucose Uptake Stimulation and α-Amylase Inhibitory Effects
Firoz Hirehal Hussain Mi, Channangihalli Thimmegowda Sadashiva, Neethumol Benny, Sreedrisya Ayippakkari Kuttiattu, Ravi Subban
International Journal of Pharmacology.2023; 19(5): 730. CrossRef - Comparison of on-Statin Lipid and Lipoprotein Levels for the Prediction of First Cardiovascular Event in Type 2 Diabetes Mellitus
Ji Yoon Kim, Jimi Choi, Sin Gon Kim, Nam Hoon Kim
Diabetes & Metabolism Journal.2023; 47(6): 837. CrossRef - Differential Impact of Obesity on the Risk of Diabetes Development in Two Age Groups: Analysis from the National Health Screening Program
Tae Kyung Yoo, Kyung-Do Han, Yang-Hyun Kim, Ga Eun Nam, Sang Hyun Park, Eun-Jung Rhee, Won-Young Lee
Diabetes & Metabolism Journal.2023; 47(6): 846. CrossRef - Strategies to Maintain the Remission of Diabetes Following Metabolic Surgery
Mi Kyung Kim, Hye Soon Kim
Journal of Metabolic and Bariatric Surgery.2023; 12(2): 26. CrossRef - East Asian perspectives in metabolic and bariatric surgery
Tae Jung Oh, Hyuk‐Joon Lee, Young Min Cho
Journal of Diabetes Investigation.2022; 13(5): 756. CrossRef - Recent Updates to Clinical Practice Guidelines for Diabetes Mellitus
Jin Yu, Seung-Hwan Lee, Mee Kyoung Kim
Endocrinology and Metabolism.2022; 37(1): 26. CrossRef - Association between Physical Exercise and Glycated Hemoglobin Levels in Korean Patients Diagnosed with Diabetes
Il Yun, Hye Jin Joo, Yu Shin Park, Eun-Cheol Park
International Journal of Environmental Research and Public Health.2022; 19(6): 3280. CrossRef - Effectiveness and safety of teneligliptin added to patients with type 2 diabetes inadequately controlled by oral triple combination therapy: A multicentre, randomized, double‐blind, and placebo‐controlled study
Minyoung Lee, Woo‐je Lee, Jae Hyeon Kim, Byung‐Wan Lee
Diabetes, Obesity and Metabolism.2022; 24(6): 1105. CrossRef - Trends of severe hypoglycemia in patients with type 2 diabetes in Korea: A longitudinal nationwide cohort study
Jae‐Seung Yun, Kyungdo Han, Seung‐Hyun Ko
Journal of Diabetes Investigation.2022; 13(8): 1438. CrossRef - GLP-1 receptor agonists in diabetic kidney disease: current evidence and future directions
Ji Hee Yu, So Young Park, Da Young Lee, Nan Hee Kim, Ji A Seo
Kidney Research and Clinical Practice.2022; 41(2): 136. CrossRef - Cardiorenal Risk Profiles Among Data-Driven Type 2 Diabetes Sub-Phenotypes: A Post-Hoc Analysis of the China Health and Nutrition Survey
Hui Gao, Kan Wang, Wensui Zhao, Jianlin Zhuang, Yu Jiang, Lei Zhang, Qingping Liu, Fariba Ahmadizar
Frontiers in Endocrinology.2022;[Epub] CrossRef - Individualized Medical Nutrition Therapy for Diabetic Patients according to Diabetes Medication
Juyeon Park
The Journal of Korean Diabetes.2022; 23(1): 50. CrossRef - Critical shear stress of red blood cells as a novel integrated biomarker for screening chronic kidney diseases in cases of type 2 diabetes
Il Rae Park, Jimi Choi, Eun Young Ha, Seung Min Chung, Jun Sung Moon, Sehyun Shin, Sin Gon Kim, Kyu Chang Won
Clinical Hemorheology and Microcirculation.2022; 81(4): 293. CrossRef - Effects of exercise on reducing diabetes risk in Korean women according to menopausal status
Jung-Hwan Cho, Hye-Mi Kwon, Se-Eun Park, Ju-Hwan Yoo, Kyung-Do Han, Eun-Jung Rhee, Won-Young Lee
Cardiovascular Prevention and Pharmacotherapy.2022; 4(2): 75. CrossRef - Novel Glycemic Index Based on Continuous Glucose Monitoring to Predict Poor Clinical Outcomes in Critically Ill Patients: A Pilot Study
Eun Yeong Ha, Seung Min Chung, Il Rae Park, Yin Young Lee, Eun Young Choi, Jun Sung Moon
Frontiers in Endocrinology.2022;[Epub] CrossRef - Free Versus Fixed-Ratio Combination of Basal Insulin and GLP-1 Receptor Agonists in Type 2 Diabetes Uncontrolled With GLP-1 Receptor Agonists: A Systematic Review and Indirect Treatment Comparison
Han Na Jung, Yun Kyung Cho, Se Hee Min, Hwi Seung Kim, Ye-Jee Kim, Joong-Yeol Park, Woo Je Lee, Chang Hee Jung
Frontiers in Endocrinology.2022;[Epub] CrossRef - Obesity, hypertension, diabetes mellitus, and hypercholesterolemia in Korean adults before and during the COVID-19 pandemic: a special report of the 2020 Korea National Health and Nutrition Examination Survey
Ga Bin Lee, Yoonjung Kim, Suyeon Park, Hyeon Chang Kim, Kyungwon Oh
Epidemiology and Health.2022; 44: e2022041. CrossRef - Adherence to healthy lifestyle behaviors as a preventable risk factor for severe hypoglycemia in people with type 2 diabetes: A longitudinal nationwide cohort study
Jae‐Seung Yun, Kyungdo Han, Yong‐Moon Park, Eugene Han, Yong‐ho Lee, Seung‐Hyun Ko
Journal of Diabetes Investigation.2022; 13(9): 1533. CrossRef - Diabetes Fact Sheet in Korea 2021
Jae Hyun Bae, Kyung-Do Han, Seung-Hyun Ko, Ye Seul Yang, Jong Han Choi, Kyung Mook Choi, Hyuk-Sang Kwon, Kyu Chang Won
Diabetes & Metabolism Journal.2022; 46(3): 417. CrossRef - Comprehensive Understanding for Application in Korean Patients with Type 2 Diabetes Mellitus of the Consensus Statement on Carbohydrate-Restricted Diets by Korean Diabetes Association, Korean Society for the Study of Obesity, and Korean Society of Hyperte
Jong Han Choi, Jee-Hyun Kang, Suk Chon
Diabetes & Metabolism Journal.2022; 46(3): 377. CrossRef - Effect of Carbohydrate-Restricted Diets and Intermittent Fasting on Obesity, Type 2 Diabetes Mellitus, and Hypertension Management: Consensus Statement of the Korean Society for the Study of Obesity, Korean Diabetes Association, and Korean Society of Hype
Jong Han Choi, Yoon Jeong Cho, Hyun-Jin Kim, Seung-Hyun Ko, Suk Chon, Jee-Hyun Kang, Kyoung-Kon Kim, Eun Mi Kim, Hyun Jung Kim, Kee-Ho Song, Ga Eun Nam, Kwang Il Kim
Diabetes & Metabolism Journal.2022; 46(3): 355. CrossRef - Effect of carbohydrate-restricted diets and intermittent fasting on obesity, type 2 diabetes mellitus, and hypertension management: consensus statement of the Korean Society for the Study of obesity, Korean Diabetes Association, and Korean Society of Hype
Jong Han Choi, Yoon Jeong Cho, Hyun-Jin Kim, Seung-Hyun Ko, Suk Chon, Jee-Hyun Kang, Kyoung-Kon Kim, Eun Mi Kim, Hyun Jung Kim, Kee-Ho Song, Ga Eun Nam, Kwang Il Kim
Clinical Hypertension.2022;[Epub] CrossRef - Efficacy of Personalized Diabetes Self-care Using an Electronic Medical Record–Integrated Mobile App in Patients With Type 2 Diabetes: 6-Month Randomized Controlled Trial
Eun Young Lee, Seon-Ah Cha, Jae-Seung Yun, Sun-Young Lim, Jin-Hee Lee, Yu-Bae Ahn, Kun-Ho Yoon, Min Kyung Hyun, Seung-Hyun Ko
Journal of Medical Internet Research.2022; 24(7): e37430. CrossRef - A double‐blind, Randomized controlled trial on glucose‐lowering EFfects and safety of adding 0.25 or 0.5 mg lobeglitazone in type 2 diabetes patients with INadequate control on metformin and dipeptidyl peptidase‐4 inhibitor therapy: REFIND study
Soree Ryang, Sang Soo Kim, Ji Cheol Bae, Ji Min Han, Su Kyoung Kwon, Young Il Kim, Il Seong Nam‐Goong, Eun Sook Kim, Mi‐kyung Kim, Chang Won Lee, Soyeon Yoo, Gwanpyo Koh, Min Jeong Kwon, Jeong Hyun Park, In Joo Kim
Diabetes, Obesity and Metabolism.2022; 24(9): 1800. CrossRef - Hypoglycemic agents and glycemic variability in individuals with type 2 diabetes: A systematic review and network meta-analysis
SuA Oh, Sujata Purja, Hocheol Shin, Minji Kim, Eunyoung Kim
Diabetes and Vascular Disease Research.2022; 19(3): 147916412211068. CrossRef - Tolerability and Effectiveness of Switching to Dulaglutide in Patients With Type 2 Diabetes Inadequately Controlled With Insulin Therapy
Youngsook Kim, Ji Hye Huh, Minyoung Lee, Eun Seok Kang, Bong-Soo Cha, Byung-Wan Lee
Frontiers in Endocrinology.2022;[Epub] CrossRef - Factors Influencing the Utilization of Diabetes Complication Tests Under the COVID-19 Pandemic: Machine Learning Approach
Haewon Byeon
Frontiers in Endocrinology.2022;[Epub] CrossRef - Association of prediabetes with death and diabetic complications in older adults: the pros and cons of active screening for prediabetes
Giwoong Choi, Hojun Yoon, Hyun Ho Choi, Kyoung Hwa Ha, Dae Jung Kim
Age and Ageing.2022;[Epub] CrossRef - Recent information on test utilization and intraindividual change in anti-glutamic acid decarboxylase antibody in Korea: a retrospective study
Rihwa Choi, Wonseo Park, Gayoung Chun, Jiwon Lee, Sang Gon Lee, Eun Hee Lee
BMJ Open Diabetes Research & Care.2022; 10(3): e002739. CrossRef - Extra-Glycemic Effects of Anti-Diabetic Medications: Two Birds with One Stone?
Eun-Jung Rhee
Endocrinology and Metabolism.2022; 37(3): 415. CrossRef - Pharmacological Treatment of Nonalcoholic Fatty Liver Disease: Antidiabetic Agents
Kyung-Soo Kim
The Journal of Korean Diabetes.2022; 23(2): 83. CrossRef - Maintaining Physical Activity Is Associated with Reduced Major Adverse Cardiovascular Events in People Newly Diagnosed with Diabetes
Duhoe Kim, Jaehun Seo, Kyoung Hwa Ha, Dae Jung Kim
Journal of Obesity & Metabolic Syndrome.2022; 31(2): 187. CrossRef - Effect of Carbohydrate-Restricted Diets and Intermittent Fasting on Obesity, Type 2 Diabetes Mellitus, and Hypertension Management: Consensus Statement of the Korean Society for the Study of Obesity, Korean Diabetes Association, and Korean Society of Hype
Jong Han Choi, Yoon Jeong Cho, Hyun-Jin Kim, Seung-Hyun Ko, Suk Chon, Jee-Hyun Kang, Kyoung-Kon Kim, Eun Mi Kim, Hyun Jung Kim, Kee-Ho Song, Ga Eun Nam, Kwang Il Kim
Journal of Obesity & Metabolic Syndrome.2022; 31(2): 100. CrossRef - Advanced Glycation End Products and Their Effect on Vascular Complications in Type 2 Diabetes Mellitus
Jeongmin Lee, Jae-Seung Yun, Seung-Hyun Ko
Nutrients.2022; 14(15): 3086. CrossRef - Severe hypoglycemia as a risk factor for cardiovascular outcomes in patients with type 2 diabetes: is it preventable?
Seung-Hyun Ko
Cardiovascular Prevention and Pharmacotherapy.2022; 4(3): 106. CrossRef - New, Novel Lipid-Lowering Agents for Reducing Cardiovascular Risk: Beyond Statins
Kyuho Kim, Henry N. Ginsberg, Sung Hee Choi
Diabetes & Metabolism Journal.2022; 46(4): 517. CrossRef - Current status of obesity treatment in Korea: based on the 2020 Korean Society for the Study of Obesity guidelines for obesity management
Eun-Jung Rhee
Journal of the Korean Medical Association.2022; 65(7): 388. CrossRef - Experiences of Using Wearable Continuous Glucose Monitors in Adults With Diabetes: A Qualitative Descriptive Study
Hee Sun Kang, Hyang Rang Park, Chun-Ja Kim, Savitri Singh-Carlson
The Science of Diabetes Self-Management and Care.2022; 48(5): 362. CrossRef - 젊은 2형 당뇨병 환자의 관리
재현 배
Public Health Weekly Report.2022; 15(35): 2474. CrossRef - Real-World Prescription Patterns and Barriers Related to the Use of Sodium-Glucose Cotransporter 2 Inhibitors among Korean Patients with Type 2 Diabetes Mellitus and Cardiovascular Disease
Jong Ha Baek, Ye Seul Yang, Seung-Hyun Ko, Kyung Do Han, Jae Hyeon Kim, Min Kyong Moon, Jong Suk Park, Byung-Wan Lee, Tae Jung Oh, Suk Chon, Jong Han Choi, Kyu Yeon Hur
Diabetes & Metabolism Journal.2022; 46(5): 701. CrossRef - Low-Density Lipoprotein Cholesterol Level, Statin Use and Myocardial Infarction Risk in Young Adults
Heekyoung Jeong, Kyungdo Han, Soon Jib Yoo, Mee Kyoung Kim
Journal of Lipid and Atherosclerosis.2022; 11(3): 288. CrossRef - Blood Pressure Target in Type 2 Diabetes Mellitus
Hyun-Jin Kim, Kwang-il Kim
Diabetes & Metabolism Journal.2022; 46(5): 667. CrossRef - Association of underweight status with the risk of tuberculosis: a nationwide population-based cohort study
Su Hwan Cho, Hyun Lee, Hyuktae Kwon, Dong Wook Shin, Hee-Kyung Joh, Kyungdo Han, Jin Ho Park, Belong Cho
Scientific Reports.2022;[Epub] CrossRef - Exploring the risk factors of impaired fasting glucose in middle-aged population living in South Korean communities by using categorical boosting machine
Haewon Byeon
Frontiers in Endocrinology.2022;[Epub] CrossRef - External validation and clinical application of the predictive model for severe hypoglycemia
Jae-Seung Yun, Kyungdo Han, Soo-Yeon Choi, Seon-Ah Cha, Yu-Bae Ahn, Seung-Hyun Ko
Frontiers in Endocrinology.2022;[Epub] CrossRef - Effect of Euonymus alatus Extracts on Diabetes Related Markers in Pancreatic β-Cells and C57BL/Ksj-db/db Mice
Ye Rin Kim, Eun-young Kim, Seong Uk Lee, Young Wan Kim, Yoon Hee Kim
Journal of the Korean Society of Food Science and Nutrition.2022; 51(9): 894. CrossRef - Muscle fat contents rather than muscle mass determines nonalcoholic steatohepatitis and liver fibrosis in patients with severe obesity
Eugene Han, Mi Kyung Kim, Hye Won Lee, Seungwan Ryu, Hye Soon Kim, Byoung Kuk Jang, Youngsung Suh
Obesity.2022; 30(12): 2440. CrossRef - Correlation between shift work and non-alcoholic fatty liver disease among male workers in the steel manufacturing company of Korea: a cross-sectional study
Kiseok Kim, Yong-Jin Lee, Soon-Chan Kwon, Young-Sun Min, Hyun Kyo Lee, Gwangin Baek, Sang Hyeon Kim, Eun-Chul Jang
Annals of Occupational and Environmental Medicine.2022;[Epub] CrossRef - FGM-based remote intervention for adults with type 1 diabetes: The FRIEND randomized clinical trial
Jinju Lee, Myeong Hoon Lee, Jiyun Park, Kyung-Soo Kim, Soo-Kyung Kim, Yong-Wook Cho, Hyun Wook Han, Young Shin Song
Frontiers in Endocrinology.2022;[Epub] CrossRef - Screening for Prediabetes and Diabetes in Korean Nonpregnant Adults: A Position Statement of the Korean Diabetes Association, 2022
Kyung Ae Lee, Dae Jung Kim, Kyungdo Han, Suk Chon, Min Kyong Moon
Diabetes & Metabolism Journal.2022; 46(6): 819. CrossRef - Blood Pressure Control in Patients with Diabetic Kidney Disease
Yaeni Kim, Won Kim, Jwa-Kyung Kim, Ju Young Moon, Samel Park, Cheol Whee Park, Hoon Suk Park, Sang Heon Song, Tae-Hyun Yoo, So-Young Lee, Eun Young Lee, Jeonghwan Lee, Kyubok Jin, Dae Ryong Cha, Jin Joo Cha, Sang Youb Han
Electrolytes & Blood Pressure.2022; 20(2): 39. CrossRef - The Gangwon Obesity and Metabolic Syndrome Study: Methods and Initial Baseline Data
Yoon Jeong Cho, Sohyun Park, Sung Soo Kim, Hyo Jin Park, Jang Won Son, Tae Kyung Lee, Sangmo Hong, Jee-Hyun Kang, Seon Mee Kim, Yang-Hyun Kim, Won Jun Kim, Young Eun Seo, Yoosuk An, Sang Youl Rhee, Suk Chon, Sookyoung Jeon, Kyungho Park, Bong-Soo Kim, Cha
Journal of Obesity & Metabolic Syndrome.2022; 31(4): 303. CrossRef - Oral Semaglutide, the First Ingestible Glucagon-Like Peptide-1 Receptor Agonist: Could It Be a Magic Bullet for Type 2 Diabetes?
Hwi Seung Kim, Chang Hee Jung
International Journal of Molecular Sciences.2021; 22(18): 9936. CrossRef - Long-term effectiveness and safety of quadruple combination therapy with empagliflozin versus dapagliflozin in patients with type 2 diabetes: 3-year prospective observational study
Eu Jeong Ku, Dong-Hwa Lee, Hyun Jeong Jeon, Tae Keun Oh
Diabetes Research and Clinical Practice.2021; 182: 109123. CrossRef - Albuminuria Is Associated with Steatosis Burden in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease (Diabetes Metab J 2021;45:698-707)
Mi-kyung Kim
Diabetes & Metabolism Journal.2021; 45(6): 968. CrossRef - Incidence and Risk Factors for Progression to Diabetes Mellitus: A Retrospective Cohort Study
Min Kyung Hyun, Jong Heon Park, Kyoung Hoon Kim, Soon-Ki Ahn, Seon Mi Ji
International Journal of Environmental Research and Public Health.2021; 19(1): 123. CrossRef - 2021 Clinical Practice Guidelines for Diabetes: Pharmacotherapy and the Korean Diabetes Association Support System
Kyu Yeon Hur
The Journal of Korean Diabetes.2021; 22(4): 250. CrossRef - 2021 Clinical Practice Guidelines for Diabetes: Management of Cardiovascular Risk
Min Kyong Moon
The Journal of Korean Diabetes.2021; 22(4): 259. CrossRef
- Impact of Subclinical Atrial Function on the Prognosis of Patients With Atrial Fibrillation and Metabolic Syndrome
- Metabolic Risk/Epidemiology
-
- Magnetic Resonance-Based Assessments Better Capture Pathophysiologic Profiles and Progression in Nonalcoholic Fatty Liver Disease
- Seung Joon Choi, Seong Min Kim, Yun Soo Kim, Oh Sang Kwon, Seung Kak Shin, Kyoung Kon Kim, Kiyoung Lee, Ie Byung Park, Cheol Soo Choi, Dong Hae Chung, Jaehun Jung, MunYoung Paek, Dae Ho Lee
- Diabetes Metab J. 2021;45(5):739-752. Published online October 28, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0137
- 8,731 View
- 219 Download
- 13 Web of Science
- 15 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 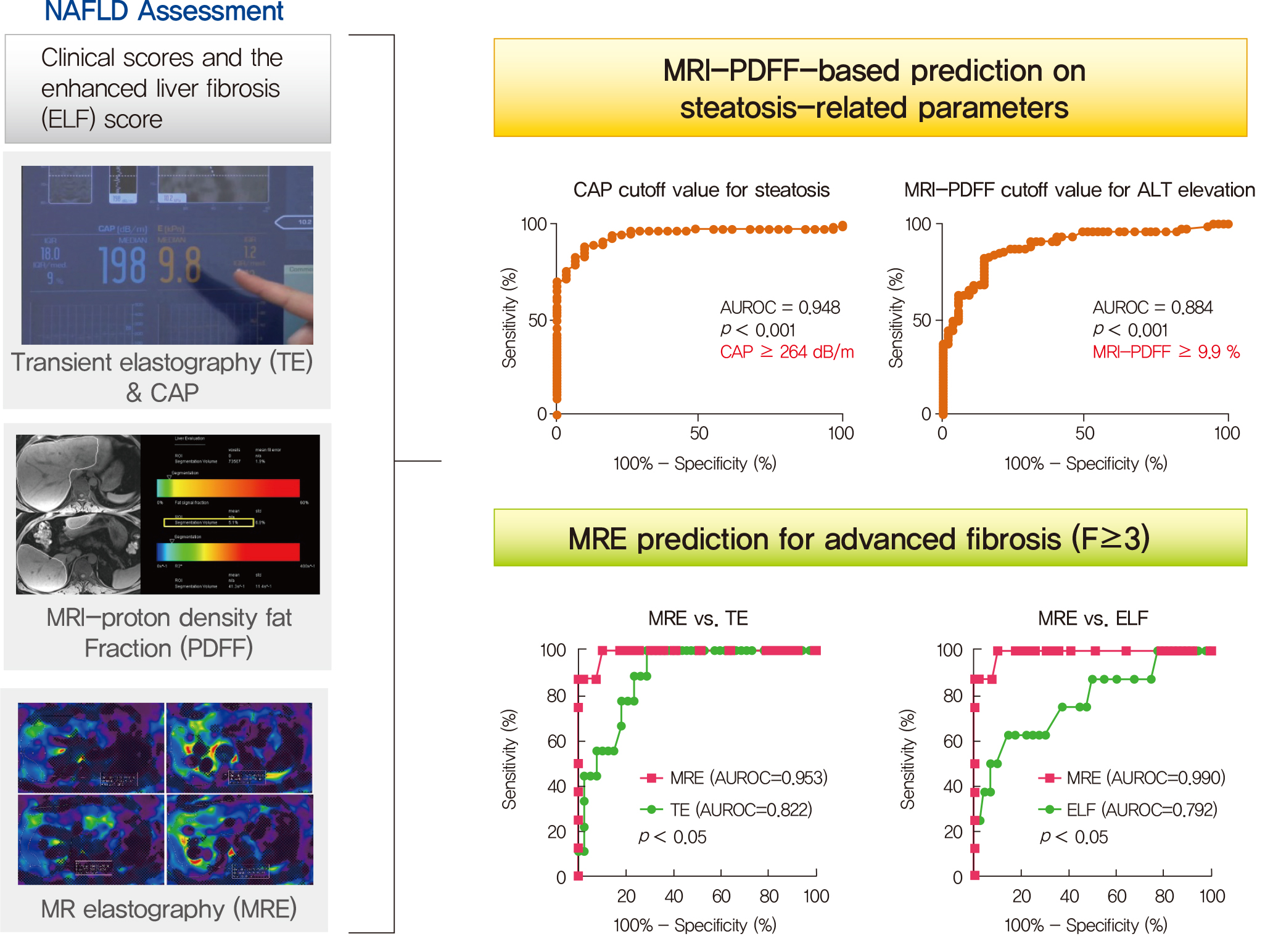
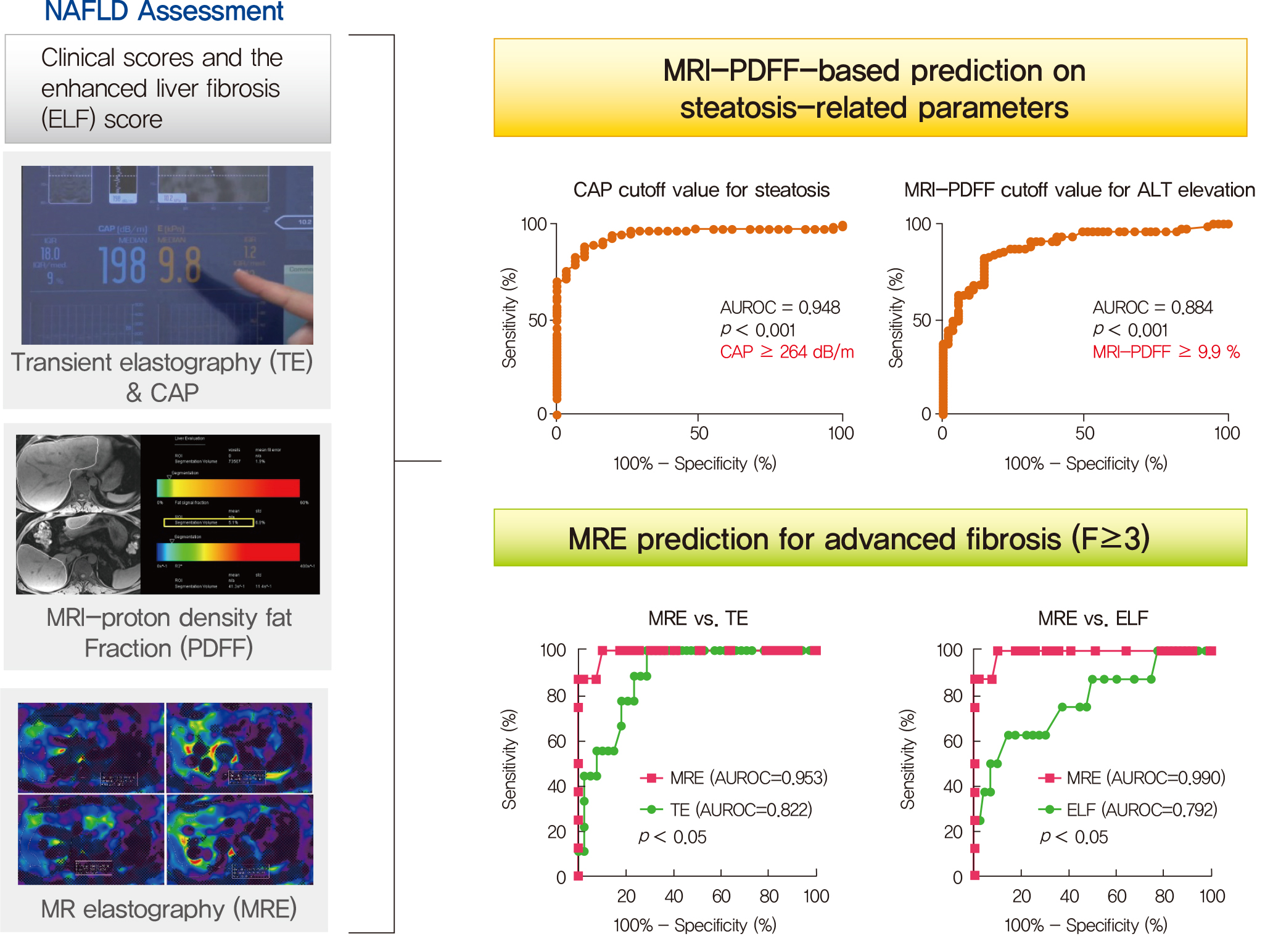
- Background
Several noninvasive tools are available for the assessment of nonalcoholic fatty liver disease (NAFLD) including clinical and blood biomarkers, transient elastography (TE), and magnetic resonance imaging (MRI) techniques, such as proton density fat fraction (MRI-PDFF) and magnetic resonance elastography (MRE). In the present study, we aimed to evaluate whether magnetic resonance (MR)-based examinations better discriminate the pathophysiologic features and fibrosis progression in NAFLD than other noninvasive methods.
Methods
A total of 133 subjects (31 healthy volunteers and 102 patients with NAFLD) were subjected to clinical and noninvasive NAFLD evaluation, with additional liver biopsy in some patients (n=54).
Results
MRI-PDFF correlated far better with hepatic fat measured by MR spectroscopy (r=0.978, P<0.001) than with the TE controlled attenuation parameter (CAP) (r=0.727, P<0.001). In addition, MRI-PDFF showed stronger correlations with various pathophysiologic parameters for cellular injury, glucose and lipid metabolism, and inflammation, than the TE-CAP. The MRI-PDFF and TE-CAP cutoff levels associated with abnormal elevation of serum alanine aminotransferase were 9.9% and 270 dB/m, respectively. The MRE liver stiffness measurement (LSM) showed stronger correlations with liver enzymes, platelets, complement component 3, several clinical fibrosis scores, and the enhanced liver fibrosis (ELF) score than the TE-LSM. In an analysis of only biopsied patients, MRE performed better in discriminating advanced fibrosis with a cutoff value of 3.9 kPa than the TE (cutoff 8.1 kPa) and ELF test (cutoff 9.2 kPa).
Conclusion
Our results suggest that MRI-based assessment of NAFLD is the best non-invasive tool that captures the histologic, pathophysiologic and metabolic features of the disease. -
Citations
Citations to this article as recorded by- A Novel Score Based on Controlled Attenuation Parameter Accurately Predicts Hepatic Steatosis in Individuals With Metabolic Dysfunction Associated Steatotic Liver Disease: A Derivation and Independent Validation Study
Zi-Ming An, Qiao-Hong Liu, Xin-Jian Ye, Qian Zhang, Hua-Fu Pei, Xin Xin, Jie Yuan, Qian Huang, Kun Liu, Fang Lu, Zhi-Han Yan, Yu Zhao, Yi-Yang Hu, Ming-Hua Zheng, Qin Feng
Clinical and Translational Gastroenterology.2024; 15(3): e00680. CrossRef - Imaging Methods Applicable in the Diagnostics of Alzheimer’s Disease, Considering the Involvement of Insulin Resistance
Petra Hnilicova, Ema Kantorova, Stanislav Sutovsky, Milan Grofik, Kamil Zelenak, Egon Kurca, Norbert Zilka, Petra Parvanovova, Martin Kolisek
International Journal of Molecular Sciences.2023; 24(4): 3325. CrossRef - Polyunsaturated and Saturated Oxylipin Plasma Levels Allow Monitoring the Non-Alcoholic Fatty Liver Disease Progression to Severe Stages
Miguel D. Ferrer, Clara Reynés, Margalida Monserrat-Mesquida, Magdalena Quetglas-Llabrés, Cristina Bouzas, Silvia García, David Mateos, Miguel Casares, Cristina Gómez, Lucía Ugarriza, Josep A. Tur, Antoni Sureda, Antoni Pons
Antioxidants.2023; 12(3): 711. CrossRef - An individual patient data meta-analysis to determine cut-offs for and confounders of NAFLD-fibrosis staging with magnetic resonance elastography
Jia-xu Liang, Javier Ampuero, Hao Niu, Kento Imajo, Mazen Noureddin, Jaideep Behari, Dae Ho Lee, Richard L. Ehman, Fredrik Rorsman, Johan Vessby, Juan R. Lacalle, Ferenc E. Mózes, Michael Pavlides, Quentin M. Anstee, Stephen A. Harrison, Javier Castell, R
Journal of Hepatology.2023; 79(3): 592. CrossRef - Relationship between controlled attenuated parameter and magnetic resonance imaging–proton density fat fraction for evaluating hepatic steatosis in patients with NAFLD
Ziming An, Qiaohong Liu, Wenli Zeng, Yan Wang, Qian Zhang, Huafu Pei, Xin Xin, Shuohui Yang, Fang Lu, Yu Zhao, Yiyang Hu, Qin Feng
Hepatology Communications.2022; 6(8): 1975. CrossRef - Noninvasive imaging of hepatic dysfunction: A state-of-the-art review
Ting Duan, Han-Yu Jiang, Wen-Wu Ling, Bin Song
World Journal of Gastroenterology.2022; 28(16): 1625. CrossRef - Diagnosis and Pathogenesis of Sarcopenia in Chronic Liver Disease Using Liver Magnetic Resonance Imaging
Atsushi Nakamura, Tsubasa Yoshimura, Tomomi Sato, Takeshi Ichikawa
Cureus.2022;[Epub] CrossRef - Plasma Aldo-Keto Reductase Family 1 Member B10 as a Biomarker Performs Well in the Diagnosis of Nonalcoholic Steatohepatitis and Fibrosis
Aron Park, Seung Joon Choi, Sungjin Park, Seong Min Kim, Hye Eun Lee, Minjae Joo, Kyoung Kon Kim, Doojin Kim, Dong Hae Chung, Jae Been Im, Jaehun Jung, Seung Kak Shin, Byung-Chul Oh, Cheolsoo Choi, Seungyoon Nam, Dae Ho Lee
International Journal of Molecular Sciences.2022; 23(9): 5035. CrossRef - Contribution of a genetic risk score to ethnic differences in fatty liver disease
Maddie J. Kubiliun, Jonathan C. Cohen, Helen H. Hobbs, Julia Kozlitina
Liver International.2022; 42(10): 2227. CrossRef - Plasma Metabolomics and Machine Learning-Driven Novel Diagnostic Signature for Non-Alcoholic Steatohepatitis
Moongi Ji, Yunju Jo, Seung Joon Choi, Seong Min Kim, Kyoung Kon Kim, Byung-Chul Oh, Dongryeol Ryu, Man-Jeong Paik, Dae Ho Lee
Biomedicines.2022; 10(7): 1669. CrossRef - Updated S2k Clinical Practice Guideline on Non-alcoholic Fatty Liver Disease (NAFLD) issued by the German Society of Gastroenterology, Digestive and Metabolic Diseases (DGVS) – April 2022 – AWMF Registration No.: 021–025
Zeitschrift für Gastroenterologie.2022; 60(09): e733. CrossRef - Aktualisierte S2k-Leitlinie nicht-alkoholische Fettlebererkrankung der Deutschen Gesellschaft für Gastroenterologie, Verdauungs- und Stoffwechselkrankheiten (DGVS) – April 2022 – AWMF-Registernummer: 021–025
E. Roeb, A. Canbay, H. Bantel, J. Bojunga, J. de Laffolie, M. Demir, U. W. Denzer, A. Geier, W. P. Hofmann, C. Hudert, T. Karlas, M. Krawczyk, T. Longerich, T. Luedde, M. Roden, J. Schattenberg, M. Sterneck, A. Tannapfel, P. Lorenz, F. Tacke
Zeitschrift für Gastroenterologie.2022; 60(09): 1346. CrossRef - Ultrasound Methods for the Assessment of Liver Steatosis: A Critical Appraisal
Dorotea Bozic, Kristian Podrug, Ivana Mikolasevic, Ivica Grgurevic
Diagnostics.2022; 12(10): 2287. CrossRef - Significance of liver fat loss in chronic liver disease: Usefulness of hepatic proton density fat fraction measurement by magnetic resonance imaging in evaluating malnutrition
Atsushi Nakamura, Haruka Okada, Tsubasa Yoshimura, Manami Deguchi, Yuei Hosokawa, Tomomi Satoh, Takeshi Ichikawa, Keiji Okuyama, Yoshihiro Yoshioka, Hitoshi Asakura
Kanzo.2021; 62(9): 525. CrossRef - Screening for nonalcoholic fatty liver disease-when, who and how?
Christoph G Dietrich, Monika Rau, Andreas Geier
World Journal of Gastroenterology.2021; 27(35): 5803. CrossRef
- A Novel Score Based on Controlled Attenuation Parameter Accurately Predicts Hepatic Steatosis in Individuals With Metabolic Dysfunction Associated Steatotic Liver Disease: A Derivation and Independent Validation Study
- Complications
- Differences in Clinical Outcomes between Patients with and without Hypoglycemia during Hospitalization: A Retrospective Study Using Real-World Evidence
- Jeongmin Lee, Tong Min Kim, Hyunah Kim, Seung-Hwan Lee, Jae Hyoung Cho, Hyunyong Lee, Hyeon Woo Yim, Kun-Ho Yoon, Hun-Sung Kim
- Diabetes Metab J. 2020;44(4):555-565. Published online May 8, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0064
- 6,531 View
- 101 Download
- 8 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub Background Some patients admitted to hospitals for glycemic control experience hypoglycemia despite regular meals and despite adhering to standard blood glucose control protocols. Different factors can have a negative impact on blood glucose control and prognosis after discharge. This study investigated risk factors for hypoglycemia and its effects on glycemic control during the hospitalization of patients in the general ward.
Methods This retrospective study included patients who were admitted between 2009 and 2018. Patients were provided regular meals at fixed times according to ideal body weights during hospitalization. We categorized the patients into two groups: those with and those without hypoglycemia during hospitalization.
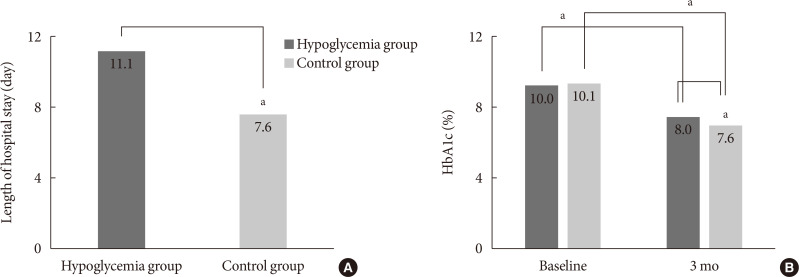
Results Of the 3,031 patients, 379 experienced at least one episode of hypoglycemia during hospitalization (HYPO group). Hypoglycemia occurred more frequently particularly in cases of premixed insulin therapy. Compared with the control group, the HYPO group was older (61.0±16.8 years vs. 59.1±16.5 years,
P =0.035), with more females (60.4% vs. 49.6%,P <0.001), lower body mass index (BMI) (23.5±4.2 kg/m2 vs. 25.1±4.4 kg/m2,P <0.001), and higher prevalence of type 1 diabetes mellitus (6.1% vs. 2.6%,P <0.001), They had longer hospital stay (11.1±13.5 days vs. 7.6±4.6 days,P <0.001). After discharge the HYPO group had lower glycosylated hemoglobin reduction rate (−2.0%±0.2% vs. −2.5%±0.1%,P =0.003) and tended to have more frequent cases of cardiovascular disease.Conclusion Hypoglycemia occurred more frequently in older female patients with lower BMI and was associated with longer hospital stay and poorer glycemic control after discharge. Therefore, clinicians must carefully ensure that patients do not experience hypoglycemia during hospitalization.
-
Citations
Citations to this article as recorded by- Acute kidney injury: a strong risk factor for hypoglycaemia in hospitalized patients with type 2 diabetes
Ana Carreira, Pedro Castro, Filipe Mira, Miguel Melo, Pedro Ribeiro, Lèlita Santos
Acta Diabetologica.2023; 60(9): 1179. CrossRef - Adherence to healthy lifestyle behaviors as a preventable risk factor for severe hypoglycemia in people with type 2 diabetes: A longitudinal nationwide cohort study
Jae‐Seung Yun, Kyungdo Han, Yong‐Moon Park, Eugene Han, Yong‐ho Lee, Seung‐Hyun Ko
Journal of Diabetes Investigation.2022; 13(9): 1533. CrossRef - Predicting hypoglycemia in hospitalized patients with diabetes: A derivation and validation study
Michal Elbaz, Jeries Nashashibi, Shiri Kushnir, Leonard Leibovici
Diabetes Research and Clinical Practice.2021; 171: 108611. CrossRef - Hospital care: improving outcomes in type 1 diabetes
Schafer Boeder, Kristen Kulasa
Current Opinion in Endocrinology, Diabetes & Obesity.2021; 28(1): 14. CrossRef - Data Pseudonymization in a Range That Does Not Affect Data Quality: Correlation with the Degree of Participation of Clinicians
Soo-Yong Shin, Hun-Sung Kim
Journal of Korean Medical Science.2021;[Epub] CrossRef - Letter: Differences in Clinical Outcomes between Patients with and without Hypoglycemia during Hospitalization: A Retrospective Study Using Real-World Evidence (Diabetes Metab J 2020;44:555-65)
Sung-Woo Kim
Diabetes & Metabolism Journal.2020; 44(5): 775. CrossRef - Response: Differences in Clinical Outcomes between Patients with and without Hypoglycemia during Hospitalization: A Retrospective Study Using Real-World Evidence (Diabetes Metab J 2020;44:555-65)
Jeongmin Lee, Hun-Sung Kim
Diabetes & Metabolism Journal.2020; 44(5): 779. CrossRef - Hypoglycaemia and Cardiovascular Disease Risk in Patients with Diabetes
Niki Katsiki, Kalliopi Kotsa, Anca P. Stoian, Dimitri P. Mikhailidis
Current Pharmaceutical Design.2020; 26(43): 5637. CrossRef
- Acute kidney injury: a strong risk factor for hypoglycaemia in hospitalized patients with type 2 diabetes
- Metabolic Risk/Epidemiology
- A Comparison of Predictive Performances between Old versus New Criteria in a Risk-Based Screening Strategy for Gestational Diabetes Mellitus
- Subeen Hong, Seung Mi Lee, Soo Heon Kwak, Byoung Jae Kim, Ja Nam Koo, Ig Hwan Oh, Sohee Oh, Sun Min Kim, Sue Shin, Won Kim, Sae Kyung Joo, Errol R. Norwitz, Souphaphone Louangsenlath, Chan-Wook Park, Jong Kwan Jun, Joong Shin Park
- Diabetes Metab J. 2020;44(5):726-736. Published online April 13, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0126
- 6,627 View
- 123 Download
- 9 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub Background The definition of the high-risk group for gestational diabetes mellitus (GDM) defined by the American College of Obstetricians and Gynecologists was changed from the criteria composed of five historic/demographic factors (old criteria) to the criteria consisting of 11 factors (new criteria) in 2017. To compare the predictive performances between these two sets of criteria.
Methods This is a secondary analysis of a large prospective cohort study of non-diabetic Korean women with singleton pregnancies designed to examine the risk of GDM in women with nonalcoholic fatty liver disease. Maternal fasting blood was taken at 10 to 14 weeks of gestation and measured for glucose and lipid parameters. GDM was diagnosed by the two-step approach.
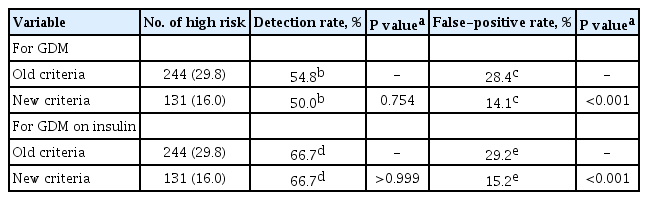
Results Among 820 women, 42 (5.1%) were diagnosed with GDM. Using the old criteria, 29.8% (
n =244) of women would have been identified as high risk versus 16.0% (n =131) using the new criteria. Of the 42 women who developed GDM, 45.2% (n =19) would have been mislabeled as not high risk by the old criteria versus 50.0% (n =21) using the new criteria (1-sensitivity, 45.2% vs. 50.0%,P >0.05). Among the 778 patients who did not develop GDM, 28.4% (n =221) would have been identified as high risk using the old criteria versus 14.1% (n =110) using the new criteria (1-specificity, 28.4% vs. 14.1%,P <0.001).Conclusion Compared with the old criteria, use of the new criteria would have decreased the number of patients identified as high risk and thus requiring early GDM screening by half (from 244 [29.8%] to 131 [16.0%]).
-
Citations
Citations to this article as recorded by- Predicting the Risk of Insulin-Requiring Gestational Diabetes before Pregnancy: A Model Generated from a Nationwide Population-Based Cohort Study in Korea
Seung-Hwan Lee, Jin Yu, Kyungdo Han, Seung Woo Lee, Sang Youn You, Hun-Sung Kim, Jae-Hyoung Cho, Kun-Ho Yoon, Mee Kyoung Kim
Endocrinology and Metabolism.2023; 38(1): 129. CrossRef - Metabolic Dysfunction-Associated Fatty Liver Disease and Subsequent Development of Adverse Pregnancy Outcomes
Seung Mi Lee, Young Mi Jung, Eun Saem Choi, Soo Heon Kwak, Ja Nam Koo, Ig Hwan Oh, Byoung Jae Kim, Sun Min Kim, Sang Youn Kim, Gyoung Min Kim, Sae Kyung Joo, Bo Kyung Koo, Sue Shin, Errol R. Norwitz, Chan-Wook Park, Jong Kwan Jun, Won Kim, Joong Shin Park
Clinical Gastroenterology and Hepatology.2022; 20(11): 2542. CrossRef - Nonalcoholic fatty liver disease and early prediction of gestational diabetes mellitus using machine learning methods
Seung Mi Lee, Suhyun Hwangbo, Errol R. Norwitz, Ja Nam Koo, Ig Hwan Oh, Eun Saem Choi, Young Mi Jung, Sun Min Kim, Byoung Jae Kim, Sang Youn Kim, Gyoung Min Kim, Won Kim, Sae Kyung Joo, Sue Shin, Chan-Wook Park, Taesung Park, Joong Shin Park
Clinical and Molecular Hepatology.2022; 28(1): 105. CrossRef - Nonalcoholic fatty liver disease-based risk prediction of adverse pregnancy outcomes: Ready for prime time?
Seung Mi Lee, Won Kim
Clinical and Molecular Hepatology.2022; 28(1): 47. CrossRef - Postprandial Free Fatty Acids at Mid-Pregnancy Increase the Risk of Large-for-Gestational-Age Newborns in Women with Gestational Diabetes Mellitus
So-Yeon Kim, Young Shin Song, Soo-Kyung Kim, Yong-Wook Cho, Kyung-Soo Kim
Diabetes & Metabolism Journal.2022; 46(1): 140. CrossRef - Effect of Different Types of Diagnostic Criteria for Gestational Diabetes Mellitus on Adverse Neonatal Outcomes: A Systematic Review, Meta-Analysis, and Meta-Regression
Fahimeh Ramezani Tehrani, Marzieh Saei Ghare Naz, Razieh Bidhendi-Yarandi, Samira Behboudi-Gandevani
Diabetes & Metabolism Journal.2022; 46(4): 605. CrossRef - Development of early prediction model for pregnancy-associated hypertension with graph-based semi-supervised learning
Seung Mi Lee, Yonghyun Nam, Eun Saem Choi, Young Mi Jung, Vivek Sriram, Jacob S. Leiby, Ja Nam Koo, Ig Hwan Oh, Byoung Jae Kim, Sun Min Kim, Sang Youn Kim, Gyoung Min Kim, Sae Kyung Joo, Sue Shin, Errol R. Norwitz, Chan-Wook Park, Jong Kwan Jun, Won Kim,
Scientific Reports.2022;[Epub] CrossRef - The Clinical Characteristics of Gestational Diabetes Mellitus in Korea: A National Health Information Database Study
Kyung-Soo Kim, Sangmo Hong, Kyungdo Han, Cheol-Young Park
Endocrinology and Metabolism.2021; 36(3): 628. CrossRef - The risk of pregnancy‐associated hypertension in women with nonalcoholic fatty liver disease
Young Mi Jung, Seung Mi Lee, Subeen Hong, Ja Nam Koo, Ig Hwan Oh, Byoung Jae Kim, Sun Min Kim, Sang Youn Kim, Gyoung Min Kim, Sae Kyung Joo, Sue Shin, Errol R. Norwitz, Chan‐Wook Park, Jong Kwan Jun, Won Kim, Joong Shin Park
Liver International.2020; 40(10): 2417. CrossRef
- Predicting the Risk of Insulin-Requiring Gestational Diabetes before Pregnancy: A Model Generated from a Nationwide Population-Based Cohort Study in Korea
- Others
- Serum R-Spondin 1 Is a New Surrogate Marker for Obesity and Insulin Resistance
- Yea Eun Kang, Ji Min Kim, Hyon-Seung Yi, Kyong Hye Joung, Ju Hee Lee, Hyun Jin Kim, Bon Jeong Ku
- Diabetes Metab J. 2019;43(3):368-376. Published online October 23, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0066
- 5,022 View
- 75 Download
- 6 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Recent
in vivo studies indicated that R-spondin 1 (RSPO1) regulates food intake and increases insulin secretion, but its role in humans remains unknown. This study investigated the association between serum levels of RSPO1 and diverse metabolic parameters in humans.Methods The study population consisted of 43 subjects with newly diagnosed diabetes mellitus, and 79 non-diabetic participants. Serum levels of RSPO1 were measured using the enzyme-linked immunosorbent assay. The relationships between circulating RSPO1 and diverse metabolic parameters were analyzed.
Results Circulating RSPO1 levels increased to a greater extent in the obese group than in the lean group. Moreover, serum levels of RSPO1 were higher in the insulin-resistant group than in the insulin-sensitive group. Serum levels of RSPO1 were significantly correlated with a range of metabolic parameters including body mass index, fasting C-peptide, homeostasis model assessment of insulin resistance index, and lipid profile. Moreover, levels were significantly associated with insulin resistance and obesity in non-diabetic subjects.
Conclusion This study demonstrated the association between serum levels of RSPO1 and a range of metabolic parameters in humans. Serum levels of RSPO1 are significantly related to obesity and insulin resistance, although the precise mechanisms remain unknown.
-
Citations
Citations to this article as recorded by- LGR4: A New Receptor Member in Endocrine and Metabolic Diseases
Ningning Zhang, Mingyang Yuan, Jiqiu Wang
Endocrine Reviews.2023; 44(4): 647. CrossRef - R-Spondin1 and tumor necrosis factor-alpha in infertile women with polycystic ovary syndrome: relationships with insulin resistance and other parameters
Tuğba GÜRBÜZ, Oya GÖKMEN, Asena AYAR MADENLİ, Berna DİLBAZ
Journal of Health Sciences and Medicine.2023; 6(2): 449. CrossRef - An early prediction model for type 2 diabetes mellitus based on genetic variants and nongenetic risk factors in a Han Chinese cohort
Jinjin Li, Qun Ye, Hongxiao Jiao, Wanyao Wang, Kai Zhang, Chen Chen, Yuan Zhang, Shuzhi Feng, Ximo Wang, Yubao Chen, Huailin Gao, Fengjiang Wei, Wei-Dong Li
Frontiers in Endocrinology.2023;[Epub] CrossRef - Emerging Therapeutic Strategies for Attenuating Tubular EMT and Kidney Fibrosis by Targeting Wnt/β-Catenin Signaling
Lichao Hu, Mengyuan Ding, Weichun He
Frontiers in Pharmacology.2022;[Epub] CrossRef - Does Serum R-Spondin-1 Play a Role in PCOS Pathophysiology?
Osman BAŞPINAR, Yasin ŞİMŞEK, Derya KOÇER, Oğuzhan Sıtkı DİZDAR, Hatice KAYIŞ TOPALOĞLU
Genel Tıp Dergisi.2022; 32(5): 490. CrossRef - Silencing of RSPO1 mitigates obesity-related renal fibrosis in mice by deactivating Wnt/β-catenin pathway
Xuesong Su, Guangyu Zhou, Mi Tian, Si Wu, Yanqiu Wang
Experimental Cell Research.2021; 405(2): 112713. CrossRef - Exosome miR‐27a‐3p secreted from adipocytes targets ICOS to promote antitumor immunity in lung adenocarcinoma
Xuehan Fan, Jingya Wang, Tingting Qin, Yujia Zhang, Wenting Liu, Kaiting Jiang, Dingzhi Huang
Thoracic Cancer.2020; 11(6): 1453. CrossRef - Integrative Analyses of Genes Associated with Subcutaneous Insulin Resistance
Manoj Kumar Pujar, Basavaraj Vastrad, Chanabasayya Vastrad
Biomolecules.2019; 9(2): 37. CrossRef
- LGR4: A New Receptor Member in Endocrine and Metabolic Diseases
- Others
- Serum Soluble Epidermal Growth Factor Receptor Level Increase in Patients Newly Diagnosed with Type 2 Diabetes Mellitus
- Ji Min Kim, Sorim Choung, Kyong Hye Joung, Ju Hee Lee, Hyun Jin Kim, Bon Jeong Ku
- Diabetes Metab J. 2018;42(4):343-347. Published online May 2, 2018
- DOI: https://doi.org/10.4093/dmj.2017.0082
- 4,324 View
- 50 Download
- 6 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader We analyzed circulating soluble epidermal growth factor receptor (sEGFR) levels in humans. Serum sEGFR levels were higher in subjects with newly diagnosed type 2 diabetes mellitus compared with controls. Serum sEGFR was positively correlated with glycosylated hemoglobin and serum glucose and negatively correlated with serum insulin and C-peptide levels.
-
Citations
Citations to this article as recorded by- Increased serum extrachromosomal circular DNA SORBS1circle level is associated with insulin resistance in patients with newly diagnosed type 2 diabetes mellitus
Xiang Kong, Shu-jun Wan, Tian-bing Chen, Lan Jiang, Yu-jie Xing, Ya-ping Bai, Qiang Hua, Xin-ming Yao, Yong-li Zhao, Hong-mei Zhang, De-guo Wang, Qing Su, Kun Lv
Cellular & Molecular Biology Letters.2024;[Epub] CrossRef - A Pilot Genome-Wide Association Study Identifies Novel Markers of Metabolic Syndrome in Patients with Psoriasis
Seung-Min Oh, Su-Kang Kim, Hye-Jin Ahn, Ki-Heon Jeong
Annals of Dermatology.2023; 35(4): 285. CrossRef - Effect of cholesterol-lowering agents on soluble epidermal growth factor receptor level in type 2 diabetes and hypercholesterolemia
Jun Choul Lee, Kyong Hye Joung, Ji Min Kim, Seon Mee Kang, Hyun Jin Kim, Bon Jeong Ku
Medicine.2022; 101(34): e30287. CrossRef - Soluble EGFR, a hepatokine, and adipsin, an adipokine, are biomarkers correlated with distinct aspects of insulin resistance in type 2 diabetes subjects
Mayu Kyohara, Jun Shirakawa, Tomoko Okuyama, Yu Togashi, Ryota Inoue, Jinghe Li, Daisuke Miyashita, Yasuo Terauchi
Diabetology & Metabolic Syndrome.2020;[Epub] CrossRef - Epidermal growth factor protects against myocardial ischaemia reperfusion injury through activating Nrf2 signalling pathway
Jun Ma, Ge Jin
Free Radical Research.2019; 53(3): 313. CrossRef
- Increased serum extrachromosomal circular DNA SORBS1circle level is associated with insulin resistance in patients with newly diagnosed type 2 diabetes mellitus
- Others
- Clinical Implications of Using Post-Challenge Plasma Glucose Levels for Early Diagnosis of Type 2 Diabetes Mellitus in Older Individuals
- Kyong Hye Joung, Sang Hyun Ju, Ji Min Kim, Sorim Choung, Jae Min Lee, Kang Seo Park, Hyun Jin Kim, Bon Jeong Ku
- Diabetes Metab J. 2018;42(2):147-154. Published online February 13, 2018
- DOI: https://doi.org/10.4093/dmj.2018.42.2.147
- 4,652 View
- 36 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The aim of this study was to explore the differences in the clinical characteristics and diagnostic rates of diabetes mellitus (DM) according to various criteria in different age groups and to evaluate the efficacy of each criterion for screening older patients.
Methods We studied 515 patients and measured the fasting plasma glucose level (FPG), 2-hour plasma glucose level after the 75 g oral glucose tolerance test (2-hour postload glucose [2-h PG]), and glycosylated hemoglobin (HbA1c) for re-evaluation of hyperglycemia without a history of diabetes. Patients with newly diagnosed DM were grouped by age as younger (<65 years) or older (≥65 years).
Results Older patients had significantly lower HbA1c, FPG, and 2-h PG levels and a higher homeostatic level of pancreatic β-cell function compared with younger patients (
P <0.001). The older group had the lowest diagnostic rate when using the FPG level (45.5%) and the highest diagnostic rate when using the 2-h PG level (84.6%). These results were mostly due to the higher frequency of isolated post-challenge hyperglycemia in the older patients than in the younger group (28.8% vs. 9.2%). The use of both the FPG and HbA1c levels significantly enhanced the low diagnostic power when employing only the FPG levels in the older group (71.2% vs. 45.5%).Conclusion In the older patients, the 2-h PG level was the most accurate diagnostic criterion. When we consider the costs and convenience, a combination of the FPG and HbA1c criteria may be recommended as a screening test for DM in older people.
-
Citations
Citations to this article as recorded by- International Diabetes Federation Position Statement on the 1-hour post-load plasma glucose for the diagnosis of intermediate hyperglycaemia and type 2 diabetes
Michael Bergman, Melania Manco, Ilhan Satman, Juliana Chan, Maria Inês Schmidt, Giorgio Sesti, Teresa Vanessa Fiorentino, Muhammad Abdul-Ghani, Ram Jagannathan, Pramod Kumar Thyparambil Aravindakshan, Rafael Gabriel, Viswanathan Mohan, Martin Buysschaert,
Diabetes Research and Clinical Practice.2024; 209: 111589. CrossRef - A unified technique for entropy enhancement based diabetic retinopathy detection using hybrid neural network
Fatima, Muhammad Imran, Anayat Ullah, Muhammad Arif, Rida Noor
Computers in Biology and Medicine.2022; 145: 105424. CrossRef - In-silico identification of peroxisome proliferator-activated receptor (PPAR)α/γ agonists from Ligand Expo Components database
Xiao-Yan Feng, Ting-Ting Ding, Ya-Ya Liu, Wei-Ren Xu, Xian-Chao Cheng
Journal of Biomolecular Structure and Dynamics.2021; 39(5): 1853. CrossRef
- International Diabetes Federation Position Statement on the 1-hour post-load plasma glucose for the diagnosis of intermediate hyperglycaemia and type 2 diabetes
- Clinical Diabetes & Therapeutics
- Effects of Lobeglitazone, a Novel Thiazolidinedione, on Bone Mineral Density in Patients with Type 2 Diabetes Mellitus over 52 Weeks
- Soo Lim, Kyoung Min Kim, Sin Gon Kim, Doo Man Kim, Jeong-Taek Woo, Choon Hee Chung, Kyung Soo Ko, Jeong Hyun Park, Yongsoo Park, Sang Jin Kim, Hak Chul Jang, Dong Seop Choi
- Diabetes Metab J. 2017;41(5):377-385. Published online October 24, 2017
- DOI: https://doi.org/10.4093/dmj.2017.41.5.377
- 4,267 View
- 42 Download
- 19 Web of Science
- 20 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The aim of this multicenter, randomized, double-blind study was to examine the effect of lobeglitazone, a novel thiazolidinedione, on the changes in bone mineral density (BMD) in patients with type 2 diabetes mellitus.
Methods A 24-week, double-blinded phase was followed by a 28-week, open-label phase, in which the placebo group also started to receive lobeglitazone. A total of 170 patients aged 34 to 76 years were randomly assigned in a 2:1 ratio to receive lobeglitazone 0.5 mg or a matching placebo orally, once daily. BMD was assessed using dual-energy X-ray absorptiometry at week 24 and at the end of the study (week 52).
Results During the double-blinded phase, the femur neck BMD showed decreasing patterns in both groups, without statistical significance (−0.85%±0.36% and −0.78%±0.46% in the lobeglitazone and placebo groups, respectively). The treatment difference between the groups was 0.07%, which was also not statistically significant. Further, minimal, nonsignificant decreases were observed in both groups in the total hip BMD compared to values at baseline, and these differences also did not significantly differ between the groups. During the open-label phase, the BMD was further decreased, but not significantly, by −0.32% at the femur neck and by −0.60% at the total hip in the lobeglitazone group, and these changes did not significantly differ compared with the original placebo group switched to lobeglitazone.
Conclusion Our results indicate that treatment with lobeglitazone 0.5 mg over 52 weeks showed no detrimental effect on the BMD compared to the placebo.
-
Citations
Citations to this article as recorded by- Efficacy and safety of novel thiazolidinedione lobeglitazone for managing type-2 diabetes a meta-analysis
Deep Dutta, Saptarshi Bhattacharya, Manoj Kumar, Priyankar K. Datta, Ritin Mohindra, Meha Sharma
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(1): 102697. CrossRef - Efficacy and safety of lobeglitazone, a new Thiazolidinedione, as compared to the standard of care in type 2 diabetes mellitus: A systematic review and meta-analysis
Shashank R. Joshi, Saibal Das, Suja Xaviar, Shambo Samrat Samajdar, Indranil Saha, Sougata Sarkar, Shatavisa Mukherjee, Santanu Kumar Tripathi, Jyotirmoy Pal, Nandini Chatterjee
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(1): 102703. CrossRef - The benefits of adipocyte metabolism in bone health and regeneration
Lisa-Marie Burkhardt, Christian H. Bucher, Julia Löffler, Charlotte Rinne, Georg N. Duda, Sven Geissler, Tim J. Schulz, Katharina Schmidt-Bleek
Frontiers in Cell and Developmental Biology.2023;[Epub] CrossRef - Will lobeglitazone rival pioglitazone? A systematic review and critical appraisal
Kalyan Kumar Gangopadhyay, Awadhesh Kumar Singh
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(4): 102747. CrossRef - Comparison of therapeutic efficacy and safety of sitagliptin, dapagliflozin, or lobeglitazone adjunct therapy in patients with type 2 diabetes mellitus inadequately controlled on sulfonylurea and metformin: Third agent study
Jun Hwa Hong, Jun Sung Moon, Kayeon Seong, Soo Lim
Diabetes Research and Clinical Practice.2023; 203: 110872. CrossRef - Bone Mineral Density Evaluation Among Type 2 Diabetic Patients in Rural Haryana, India: An Analytical Cross-Sectional Study
Nitish Khandelwal, Surbhi Rajauria, Siddhesh Pandurang Kanjalkar, Omkar Shivaji Chavanke, Sanjay Rai
Cureus.2023;[Epub] CrossRef - Lobeglitazone and Its Therapeutic Benefits: A Review
Balamurugan M, Sarumathy S, Robinson R
Cureus.2023;[Epub] CrossRef - A double‐blind, Randomized controlled trial on glucose‐lowering EFfects and safety of adding 0.25 or 0.5 mg lobeglitazone in type 2 diabetes patients with INadequate control on metformin and dipeptidyl peptidase‐4 inhibitor therapy: REFIND study
Soree Ryang, Sang Soo Kim, Ji Cheol Bae, Ji Min Han, Su Kyoung Kwon, Young Il Kim, Il Seong Nam‐Goong, Eun Sook Kim, Mi‐kyung Kim, Chang Won Lee, Soyeon Yoo, Gwanpyo Koh, Min Jeong Kwon, Jeong Hyun Park, In Joo Kim
Diabetes, Obesity and Metabolism.2022; 24(9): 1800. CrossRef - A Real-World Study of Long-Term Safety and Efficacy of Lobeglitazone in Korean Patients with Type 2 Diabetes Mellitus
Bo-Yeon Kim, Hyuk-Sang Kwon, Suk Kyeong Kim, Jung-Hyun Noh, Cheol-Young Park, Hyeong-Kyu Park, Kee-Ho Song, Jong Chul Won, Jae Myung Yu, Mi Young Lee, Jae Hyuk Lee, Soo Lim, Sung Wan Chun, In-Kyung Jeong, Choon Hee Chung, Seung Jin Han, Hee-Seok Kim, Ju-Y
Diabetes & Metabolism Journal.2022; 46(6): 855. CrossRef - Comparative Efficacy of Lobeglitazone Versus Pioglitazone on Albuminuria in Patients with Type 2 Diabetes Mellitus
Kyung-Soo Kim, Sangmo Hong, Hong-Yup Ahn, Cheol-Young Park
Diabetes Therapy.2021; 12(1): 171. CrossRef - Lobeglitazone: A Novel Thiazolidinedione for the Management of Type 2 Diabetes Mellitus
Jaehyun Bae, Taegyun Park, Hyeyoung Kim, Minyoung Lee, Bong-Soo Cha
Diabetes & Metabolism Journal.2021; 45(3): 326. CrossRef - Effect of lobeglitazone on motor function in rat model of Parkinson’s disease with diabetes co-morbidity
Kambiz Hassanzadeh, Arman Rahimmi, Mohammad Raman Moloudi, Rita Maccarone, Massimo Corbo, Esmael Izadpanah, Marco Feligioni
Brain Research Bulletin.2021; 173: 184. CrossRef - Recent Perspective on Thiazolidinedione
Won Jun Kim
The Journal of Korean Diabetes.2021; 22(2): 97. CrossRef - Use of in vitro bone models to screen for altered bone metabolism, osteopathies, and fracture healing: challenges of complex models
Sabrina Ehnert, Helen Rinderknecht, Romina H. Aspera-Werz, Victor Häussling, Andreas K. Nussler
Archives of Toxicology.2020; 94(12): 3937. CrossRef - Update on: effects of anti-diabetic drugs on bone metabolism
Guillaume Mabilleau, Béatrice Bouvard
Expert Review of Endocrinology & Metabolism.2020; 15(6): 415. CrossRef - The use of metformin, insulin, sulphonylureas, and thiazolidinediones and the risk of fracture: Systematic review and meta‐analysis of observational studies
Khemayanto Hidayat, Xuan Du, Meng‐Jiao Wu, Bi‐Min Shi
Obesity Reviews.2019; 20(10): 1494. CrossRef - Diabetes pharmacotherapy and effects on the musculoskeletal system
Evangelia Kalaitzoglou, John L. Fowlkes, Iuliana Popescu, Kathryn M. Thrailkill
Diabetes/Metabolism Research and Reviews.2019;[Epub] CrossRef - Morin Exerts Anti‐Arthritic Effects by Attenuating Synovial Angiogenesis via Activation of Peroxisome Proliferator Activated Receptor‐γ
Mengfan Yue, Ni Zeng, Yufeng Xia, Zhifeng Wei, Yue Dai
Molecular Nutrition & Food Research.2018;[Epub] CrossRef - The effects of diabetes therapy on bone: A clinical perspective
Karim G. Kheniser, Carmen M. Polanco Santos, Sangeeta R. Kashyap
Journal of Diabetes and its Complications.2018; 32(7): 713. CrossRef - Changes in the Bone Mineral Density of Femur Neck and Total Hip Over a 52-Week Treatment with Lobeglitazone
Da Young Lee, Ji A Seo
Diabetes & Metabolism Journal.2017; 41(5): 374. CrossRef
- Efficacy and safety of novel thiazolidinedione lobeglitazone for managing type-2 diabetes a meta-analysis
- Clinical Care/Education
- Physician-Directed Diabetes Education without a Medication Change and Associated Patient Outcomes
- Hun-Sung Kim, Hyunah Kim, Hae-Kyung Yang, Eun Young Lee, Yoo Jin Jeong, Tong Min Kim, So Jung Yang, Seo Yeon Baik, Seung-Hwan Lee, Jae Hyoung Cho, In Young Choi, Hyeon Woo Yim, Bong-Yun Cha
- Diabetes Metab J. 2017;41(3):187-194. Published online May 12, 2017
- DOI: https://doi.org/10.4093/dmj.2017.41.3.187
- 4,343 View
- 38 Download
- 1 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background When patients with diabetes mellitus (DM) are first referred to a hospital from primary health care clinics, physicians have to decide whether to administer an oral hypoglycemic agent (OHA) immediately or postpone a medication change in favor of diabetes education regarding diet or exercise. The aim of this study was to determine the effect of diabetes education alone (without alterations in diabetes medication) on blood glucose levels.
Methods The study was conducted between January 2009 and December 2013 and included patients with DM. The glycosylated hemoglobin (HbA1c) levels were evaluated at the first visit and after 3 months. During the first medical examination, a designated doctor also conducted a diabetes education session that mainly covered dietary management.
Results Patients were divided into those who received no diabetic medications (
n =66) and those who received an OHA (n =124). Education resulted in a marked decrease in HbA1c levels in the OHA group among patients who had DM for <1 year (from 7.0%±1.3% to 6.6%±0.9%,P =0.0092) and for 1 to 5 years (from 7.5%±1.8% to 6.9%±1.1%,P =0.0091). Those with DM >10 years showed a slightly lower HbA1c target achievement rate of <6.5% (odds ratio, 0.089;P =0.0024).Conclusion For patients who had DM for more than 5 years, higher doses or changes in medication were more effective than intensive active education. Therefore, individualized and customized education are needed for these patients. For patients with a shorter duration of DM, it may be more effective to provide initial intensive education for diabetes before prescribing medicines, such as OHAs.
-
Citations
Citations to this article as recorded by- Management Status of Patients with Type 2 Diabetes Mellitus at General Hospitals in Korea: A 5-Year Follow-Up Study
Jin Hee Jung, Jung Hwa Lee, Hyang Mi Jang, Young Na, Hee Sun Choi, Yeon Hee Lee, Yang Gyo Kang, Na Rae Kim, Jeong Rim Lee, Bok Rye Song, Kang Hee Sim
The Journal of Korean Diabetes.2022; 23(1): 64. CrossRef - Effect of Voluntary Participation on Mobile Health Care in Diabetes Management: Randomized Controlled Open-Label Trial
Da Young Lee, Seung-Hyun Yoo, Kyong Pil Min, Cheol-Young Park
JMIR mHealth and uHealth.2020; 8(9): e19153. CrossRef - Developing a multi-center clinical data mart of ACEI and ARB for real-world evidence (RWE)
Hun-Sung Kim, Sue Hyun Lee, Tong Min Kim, Ju Han Kim
Clinical Hypertension.2018;[Epub] CrossRef
- Management Status of Patients with Type 2 Diabetes Mellitus at General Hospitals in Korea: A 5-Year Follow-Up Study
- Epidemiology
- Application of the 2013 American College of Cardiology/American Heart Association Cholesterol Guideline to the Korean National Health and Nutrition Examination Surveys from 1998 to 2012
- Young Shin Song, Tae Jung Oh, Kyoung Min Kim, Jae Hoon Moon, Sung Hee Choi, Hak Chul Jang, Kyong Soo Park, Soo Lim
- Diabetes Metab J. 2017;41(1):38-50. Published online December 16, 2016
- DOI: https://doi.org/10.4093/dmj.2017.41.1.38
- 4,285 View
- 29 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background The 2013 American College of Cardiology/American Heart Association (ACC/AHA) guideline for the treatment of blood cholesterol recommends statin therapy for individuals at high risk of atherosclerotic cardiovascular disease (ASCVD). The aim of this study was to investigate serial trends in the percentages of Korean adults considered eligible for statin therapy according to the new ACC/AHA cholesterol guideline.
Methods Data from the Korean National Health and Nutrition Examination Survey (KNHANES) I (1998,
n =7,698), II (2001,n =5,654), III (2005,n =5,269), IV (2007 to 2009,n =15,727), and V (2010 to 2012,n =16,304), which used a stratified, multistage, probability sampling design, were used as representative of the entire Korean population.Results The percentage of adults eligible for statin therapy according to the ACC/AHA cholesterol guideline increased with time: 17.0%, 19.0%, 20.8%, 20.2%, and 22.0% in KNHANES I, II, III, IV, and V, respectively (
P =0.022). The prevalence of ASCVD was 1.4% in KNHANES I and increased to 3.3% in KNHANES V. The percentage of diabetic patients aged 40 to 75 years with a low density lipoprotein cholesterol levels of 70 to 189 mg/dL increased from 4.8% in KNHANES I to 6.1% in KNHANES V. People with an estimated 10-year ASCVD risk ≥7.5% and aged 40 to 75 years accounted for the largest percentage among the four statin benefit groups: 9.1% in KNHANES I and 11.0% in KNHANES V.Conclusion Application of the 2013 ACC/AHA guideline has found that the percentage of Korean adults in the statin benefit groups has increased over the past 15 years.
-
Citations
Citations to this article as recorded by- Sex differences in risk factors for subclinical hypothyroidism
Jeonghoon Ha, Jeongmin Lee, Kwanhoon Jo, Dong-Jun Lim, Moo Il Kang, Bong Yun Cha, Min-Hee Kim
Endocrine Connections.2018; 7(4): 511. CrossRef
- Sex differences in risk factors for subclinical hypothyroidism
- Clinical Care/Education
- Factors Associated with Participation in Diabetes Education: The Korea National Health and Nutrition Examination Survey 2007 to 2009
- Jung Min Kim, Jae Won Hong, Jung Hyun Noh, Dong-Jun Kim
- Diabetes Metab J. 2016;40(6):447-453. Published online September 20, 2016
- DOI: https://doi.org/10.4093/dmj.2016.40.6.447
- 4,141 View
- 34 Download
- 8 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background A recent study revealed that the participation rate in diabetes education among diabetic patients was only about 50% in Korea. We investigated the factors associated with participation in diabetes education.
Methods The study included 1,255 patients (≥19 years old) diagnosed with diabetes drawn from the total Korea National Health and Nutrition Examination Survey 2007 to 2009 population comprising 30,705 individuals. We compared age, sex, and age- and sex-adjusted clinical characteristics in patients who had received diabetes education versus those who had not.
Results Of the 1,255 patients, 19.8% (
n =248) had received diabetes education. Patients in the group who received diabetes education were younger, diagnosed at an earlier age, had a longer diabetes duration and were more likely to be using insulin therapy compared with the group who did not receive diabetes education (P <0.001). The group who received diabetes education included fewer manual workers (P <0.001) but more college graduates (P =0.004) compared with the group who did not receive diabetes education. Logistic regression analysis revealed that longer diabetes duration increased the likelihood of receiving diabetes education (odds ratio [OR], 1.04; 95% confidence interval [CI], 1.01 to 1.06;P =0.004). Junior high school (OR, 0.47; 95% CI, 0.24 to 0.91;P =0.026) and elementary school education levels (OR, 0.34; 95% CI, 0.17 to 0.65;P =0.001) versus college graduation were inversely correlated with participation in diabetes self-management education. Non-insulin therapy reduced the likelihood of receiving diabetes education (OR, 0.37; 95% CI, 0.21 to 0.64;P <0.001).Conclusion Longer diabetes duration, insulin therapy, and higher education level were positively associated with the completion of diabetes education.
-
Citations
Citations to this article as recorded by- Management Status of Patients with Type 2 Diabetes Mellitus at General Hospitals in Korea: A 5-Year Follow-Up Study
Jin Hee Jung, Jung Hwa Lee, Hyang Mi Jang, Young Na, Hee Sun Choi, Yeon Hee Lee, Yang Gyo Kang, Na Rae Kim, Jeong Rim Lee, Bok Rye Song, Kang Hee Sim
The Journal of Korean Diabetes.2022; 23(1): 64. CrossRef - Team-based multicomponent care improved and sustained glycaemic control in obese people with type 2 diabetes (T2D) in a Diabetes Centre setting: A quality improvement program with quasi-experimental design
Lee-Ling Lim, Eric S.H. Lau, Risa Ozaki, Tammy T.Y. So, Rebecca Y.M. Wong, Elaine Y.K. Chow, Ronald C.W. Ma, Andrea O.Y. Luk, Juliana C.N. Chan, Alice P.S. Kong
Diabetes Research and Clinical Practice.2022; 194: 110138. CrossRef - Socio-economic determinants of attendance at diabetes self-management education program: using Andersen’s behavioral model
Javad Javan-Noughabi, Seyed Saeed Tabatabaee, Sajad Vahedi, Tahere Sharifi
BMC Health Services Research.2022;[Epub] CrossRef - Sociodemographic Factors Associated with Participation in Diabetes Education among Community-Dwelling Adults with Diabetes
Young-Hoon Lee
Yonsei Medical Journal.2020; 61(2): 169. CrossRef - Influence of health education on clinical parameters in type 2 diabetic subjects with and without hypertension: A longitudinal, comparative analysis in routine primary care settings
Xiu-Jing Hu, Hua-Feng Wu, Yu-Ting Li, Yi Wang, Hui Cheng, Jia-Ji Wang, Bedru H. Mohammed, Isabella Tan, Harry H.X. Wang
Diabetes Research and Clinical Practice.2020; 170: 108539. CrossRef - Disparities in Diabetes Education Program Use by Disability Status Among People with Diabetes: Findings from Behavioral Risk Factor Surveillance System 2015
Junrong Shi, Yong Li
American Journal of Health Education.2019; 50(1): 6. CrossRef - Factors Influencing Preferences of Adults With Type 2 Diabetes for Diabetes Self-Management Education Interventions
Lifeng Fan, Souraya Sidani
Canadian Journal of Diabetes.2018; 42(6): 645. CrossRef - Antihyperglycemic agent therapy for adult patients with type 2 diabetes mellitus 2017: a position statement of the Korean Diabetes Association
Seung-Hyun Ko, Kyu-Yeon Hur, Sang Youl Rhee, Nan-Hee Kim, Min Kyong Moon, Seok-O Park, Byung-Wan Lee, Hyun Jin Kim, Kyung Mook Choi, Jin Hwa Kim
The Korean Journal of Internal Medicine.2017; 32(6): 947. CrossRef - Antihyperglycemic Agent Therapy for Adult Patients with Type 2 Diabetes Mellitus 2017: A Position Statement of the Korean Diabetes Association
Seung-Hyun Ko, Kyu-Yeon Hur, Sang Youl Rhee, Nan-Hee Kim, Min Kyong Moon, Seok-O Park, Byung-Wan Lee, Hyun Jin Kim, Kyung Mook Choi, Jin Hwa Kim
Diabetes & Metabolism Journal.2017; 41(5): 337. CrossRef
- Management Status of Patients with Type 2 Diabetes Mellitus at General Hospitals in Korea: A 5-Year Follow-Up Study

 KDA
KDA
 First
First Prev
Prev





